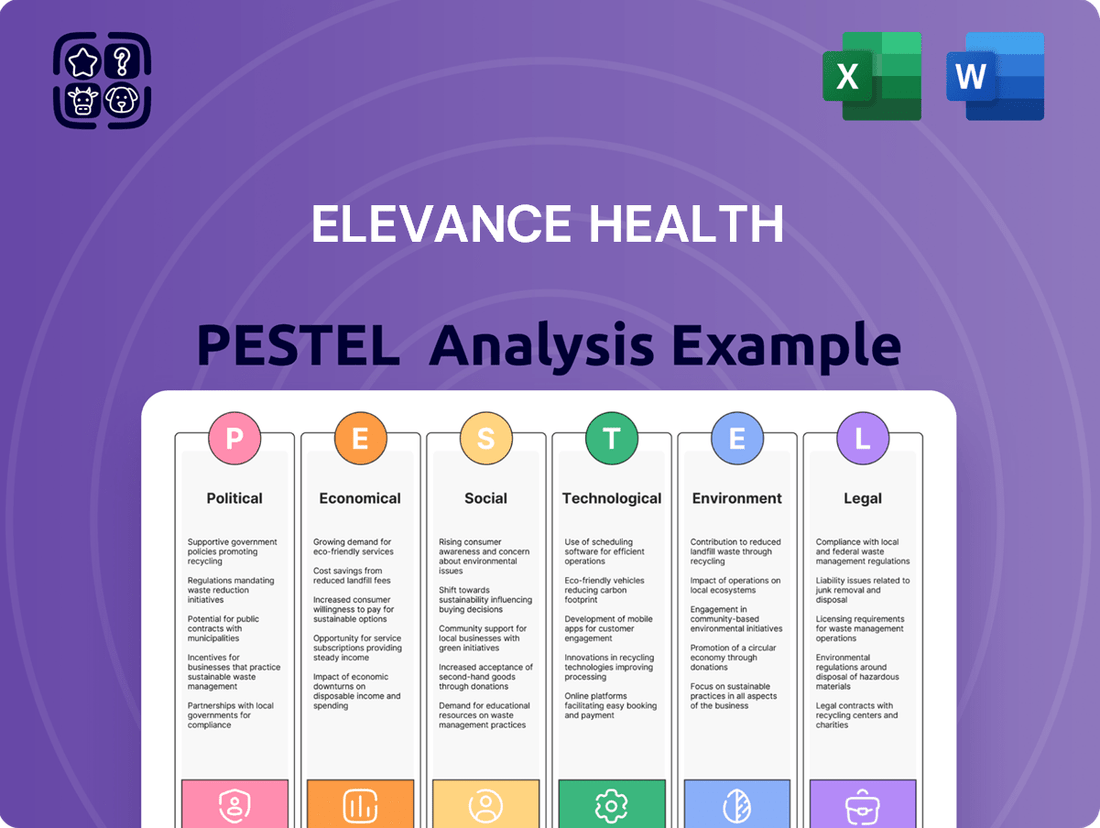
Elevance Health PESTLE Analysis
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
Elevance Health Bundle
Navigating the complex healthcare landscape requires a deep understanding of external forces. Our PESTLE analysis of Elevance Health meticulously unpacks the political, economic, social, technological, legal, and environmental factors shaping its strategic direction. Discover how evolving regulations, economic shifts, and societal trends present both challenges and opportunities for Elevance Health. Gain a competitive edge by leveraging these critical insights. Download the full PESTLE analysis now for actionable intelligence to inform your own strategic planning.
Political factors
Changes in government programs like Medicare Advantage and Medicaid significantly shape the US healthcare market, a key area for Elevance Health. Fluctuations in reimbursement rates, eligibility rules, and funding directly affect Elevance's membership numbers and financial performance.
For example, the proposed 2025 Budget Reconciliation Act's significant spending reductions for Medicaid could impact coverage for millions, potentially leading to membership declines for health insurers like Elevance.
The Affordable Care Act (ACA) marketplaces are a dynamic landscape, and changes here directly affect major health insurers like Elevance Health. These shifts can influence how many people enroll and the overall cost of coverage.
Elevance Health has faced increased costs within the ACA markets, and a slower adjustment of rates in Medicaid programs. This financial pressure prompted Elevance Health to adjust its 2025 earnings forecast downwards, signaling continued challenges in these areas.
Looking ahead, potential policy shifts, such as the expiration of expanded ACA subsidies and new rules for eligibility and enrollment, could significantly reshape the ACA market. These changes introduce a layer of uncertainty for insurers operating within these exchanges.
The telehealth regulatory landscape is in flux. Federal agencies like the DEA and HHS have extended certain flexibilities until December 31, 2025, providing a window for new regulations. This extension is crucial for providers and payers alike as they adapt to evolving virtual care standards.
However, the Centers for Medicare & Medicaid Services (CMS) is slated to revert to pre-pandemic telehealth policies. This shift could restrict patient access to virtual care, particularly for Medicare beneficiaries, unless Congress enacts new legislation. For instance, the removal of certain waivers could impact the reimbursement for specific telehealth services, affecting revenue streams for healthcare providers.
These policy developments directly impact Elevance Health's digital health initiatives and how it delivers care. The company must navigate these changes to ensure continued service delivery and patient engagement in a dynamic virtual care environment. For example, Elevance Health's investment in its own telehealth platform, Carelon Digital Office, is directly influenced by these regulatory shifts.
Healthcare Spending and Value Initiatives
Political pressure to control healthcare costs and enhance value for money remains a significant factor influencing Elevance Health. The company actively addresses this by implementing innovative care models and value-based delivery systems. This strategic approach is designed to manage escalating healthcare expenditures and streamline the member experience, directly supporting policy shifts towards outcome-based reimbursement over traditional fee-for-service models.
Elevance Health's commitment to value-based care is demonstrated through its focus on preventative services and managing chronic conditions, aiming to reduce overall healthcare utilization and costs. For instance, in 2024, the company highlighted its efforts in expanding access to primary care and behavioral health services, which are key components of value-based initiatives. By focusing on member health outcomes, Elevance aims to align its financial performance with societal goals of a more efficient and effective healthcare system.
- Government Mandates: Political bodies frequently introduce regulations impacting healthcare provider reimbursement and coverage, directly influencing Elevance Health's operational strategies.
- Value-Based Care Push: Policy incentives encourage a transition from fee-for-service to payment models tied to patient outcomes and quality of care.
- Cost Containment Efforts: Political discourse and legislative actions often target reducing overall healthcare spending, pushing insurers like Elevance to find cost-effective solutions.
- Public Health Initiatives: Government-led public health campaigns and preventive care programs can create opportunities for Elevance to partner and align its services.
Reproductive Health Policy and State Autonomy
The political landscape surrounding reproductive health is a significant factor for Elevance Health, with ongoing shifts impacting insurance coverage and provider networks. A recent federal court decision nullified a HIPAA Privacy Rule amendment designed to enhance the privacy of reproductive health information. This ruling could create complexities in data management and patient privacy protocols for insurers.
Looking ahead to June 2025, a Supreme Court decision may grant states the authority to limit Medicaid reimbursements to specific providers, including those offering abortion services. This potential change could directly affect Elevance Health's operational capacity and member access in states that choose to implement such restrictions. For instance, if a state were to ban Medicaid funding for certain reproductive services, it could necessitate adjustments to Elevance's provider contracts and member benefit structures.
- Federal actions: Recent judicial decisions have altered the regulatory environment for reproductive health information privacy.
- State autonomy: A June 2025 Supreme Court ruling might empower states to restrict Medicaid payments to certain reproductive health providers.
- Impact on insurers: These policy shifts can influence Elevance Health's network management, member access, and compliance requirements.
- Financial implications: Changes in reimbursement policies could affect revenue streams and operational costs for health insurance providers.
Government policies on Medicare Advantage and Medicaid are pivotal for Elevance Health, influencing membership and revenue. For instance, the company adjusted its 2025 earnings forecast downwards due to increased costs in ACA markets and slower Medicaid rate adjustments, highlighting financial pressures.
The evolving telehealth regulatory landscape, with flexibilities extended until December 31, 2025, but a planned reversion to pre-pandemic CMS policies, presents both opportunities and challenges for Elevance's digital health strategies.
Political pressure to control healthcare costs drives Elevance's focus on value-based care models, emphasizing preventative services and chronic condition management to improve outcomes and reduce overall spending.
Shifts in reproductive health policy, including recent court decisions impacting privacy rules and potential state authority over Medicaid reimbursements, create complexities for Elevance's network management and member access.
| Policy Area | Impact on Elevance Health | Key Developments (2024-2025) |
|---|---|---|
| Government Programs (Medicare/Medicaid) | Membership & Revenue Fluctuations | Adjusted 2025 earnings forecast due to Medicaid rate lags. |
| Telehealth Regulation | Digital Health Strategy & Service Delivery | Flexibilities extended to Dec 31, 2025; planned reversion to pre-pandemic CMS policies. |
| Healthcare Cost Containment | Operational Strategy & Value-Based Care Adoption | Focus on preventative care and chronic condition management. |
| Reproductive Health Policy | Network Management & Member Access | Impacted by privacy rule changes and potential state Medicaid reimbursement restrictions. |
What is included in the product
This PESTLE analysis delves into the Political, Economic, Social, Technological, Environmental, and Legal factors impacting Elevance Health, offering a comprehensive view of its operating landscape.
It provides actionable insights for strategic decision-making, highlighting how these macro-environmental forces create both challenges and avenues for growth within the healthcare sector.
This PESTLE analysis for Elevance Health offers a clear, summarized version of external factors, simplifying complex market dynamics for efficient stakeholder discussions and strategic decision-making.
Economic factors
Elevance Health's financial health is closely tied to healthcare cost trends, especially within its Medicaid and Affordable Care Act (ACA) segments. These rising medical costs directly impact the company's ability to maintain profitability.
The company specifically pointed to higher medical cost trends in Medicaid and increased expenses in the ACA marketplaces as reasons for a dip in its operating margin. This led to a downward revision of its 2025 earnings forecast, highlighting the sensitivity of its performance to these cost pressures.
For instance, in the first quarter of 2024, Elevance Health reported that its medical cost ratio, a key indicator of healthcare spending, was higher than anticipated. This trend necessitates a strong focus on cost management strategies to ensure continued growth and financial stability.
The health insurance sector is intensely competitive, with numerous companies battling for customer acquisition and retention. Elevance Health navigates this landscape by emphasizing a holistic approach to health and sustainable business models, aiming to meet changing consumer demands.
A key factor for Elevance Health's success is its capacity for competitive pricing and effective management of its medical loss ratio. For instance, in the first quarter of 2024, Elevance Health reported a medical revenue of $56.6 billion, demonstrating the scale of operations within this competitive market.
Health insurers like Elevance Health rely on investment income, often from fixed-income securities, making them sensitive to interest rate fluctuations. While rising inflation might eventually benefit insurers with longer-term provider contracts, a prolonged period of low interest rates can indeed dampen their investment earnings, creating a headwind. For instance, as of early 2024, the Federal Reserve's benchmark interest rate remained elevated compared to previous years, offering a more favorable environment for investment income than a scenario with persistently low rates.
Elevance Health's financial resilience is bolstered by its robust balance sheets and consistent operating cash flows, providing a degree of insulation against market volatility. This financial strength allows the company to navigate periods of fluctuating interest rates and economic uncertainty more effectively. Their ability to generate strong operating cash flow, which was reported in the billions for recent fiscal years, supports their investment strategies and overall financial flexibility.
Economic Slowdown and Disposable Income
Economic slowdowns directly influence consumer spending power, impacting Elevance Health's membership growth. A decrease in disposable income can lead individuals to opt for less comprehensive, lower-cost health insurance plans or even forgo coverage altogether, particularly in the commercial and individual market segments. For instance, if inflation continues to pressure household budgets through 2024 and into 2025, consumers may re-evaluate their healthcare spending priorities.
Elevance Health's diversified business model, encompassing various health insurance products and services, provides a degree of resilience against these economic headwinds. By offering a broad spectrum of plans, from high-deductible options to more comprehensive coverage, the company can cater to a wider range of customer affordability levels. This strategy helps to cushion the impact of reduced disposable income on overall membership numbers.
- Impact on Affordability: Rising inflation and potential economic slowdowns in 2024-2025 could reduce household disposable income, making health insurance premiums a greater burden for many consumers.
- Membership Growth Concerns: A decline in disposable income may lead to decreased enrollment in commercial and individual health insurance plans, directly affecting Elevance Health's membership growth targets.
- Plan Selection Shifts: Consumers facing tighter budgets are likely to favor more affordable, potentially less comprehensive health plans, influencing the mix of products sold by Elevance Health.
- Diversification as a Mitigator: Elevance Health's broad portfolio across different insurance segments and plan types helps to offset the risks associated with a downturn in any single market.
Impact of High-Cost Therapies
The swift approval of novel, high-priced specialty drugs, particularly cell and gene therapies, presents a substantial financial hurdle for health insurers like Elevance Health. These advanced treatments, while offering groundbreaking medical advancements, can dramatically inflate overall medical expenditures.
For instance, some gene therapies approved in recent years carry price tags exceeding $2 million per treatment, directly impacting insurers' medical cost ratios. This trend necessitates proactive financial management strategies to maintain profitability and affordability for members.
Elevance Health, like other major payers, is actively investigating and implementing sophisticated risk management techniques. These include exploring multi-pronged reinsurance strategies to mitigate the financial exposure associated with these exceptionally costly therapies.
- High-Cost Drug Approvals: The increasing number of specialty drugs with price tags in the hundreds of thousands to millions of dollars is a growing concern.
- Impact on Medical Expenses: These therapies can significantly increase a health insurer's benefit expense ratio, affecting overall financial performance.
- Reinsurance Strategies: Insurers are looking at reinsurance as a key tool to transfer some of the financial risk associated with these outlier medical costs.
- Market Dynamics: The pharmaceutical industry's focus on developing and pricing these innovative, albeit expensive, treatments directly influences the economic landscape for healthcare payers.
Economic factors significantly shape Elevance Health's operational landscape, particularly concerning healthcare costs and consumer affordability. Rising medical costs, especially within Medicaid and ACA segments, directly pressure profitability, as evidenced by Elevance's downward revision of its 2025 earnings forecast due to higher medical cost trends in Q1 2024. Economic slowdowns and inflation can reduce consumer spending power, potentially impacting membership growth and shifting plan preferences towards more affordable options, though Elevance's diversified model offers some mitigation. Furthermore, the financial sector's sensitivity to interest rates means that while elevated rates in early 2024 benefited investment income, persistent low rates could dampen earnings.
Same Document Delivered
Elevance Health PESTLE Analysis
The preview shown here is the exact document you’ll receive after purchase—fully formatted and ready to use. This comprehensive Elevance Health PESTLE analysis delves into the Political, Economic, Social, Technological, Legal, and Environmental factors impacting the company. Gain immediate access to this insightful report upon purchase.
Sociological factors
The increasing number of older adults, a demographic inherently more susceptible to complex health issues and requiring more frequent medical attention, directly fuels demand for healthcare services and specialized insurance. This trend is amplified by the rising prevalence of chronic diseases, which significantly impacts healthcare utilization and insurance pricing strategies.
In 2024, projections indicate that individuals aged 65 and over will represent a substantial portion of the population, driving a continuous need for chronic disease management and preventative care. Elevance Health's strategic emphasis on Medicare Advantage plans, which offer comprehensive coverage tailored to the needs of seniors, positions it favorably to capitalize on this demographic shift, as evidenced by their continued growth in this segment.
Elevance Health champions a holistic 'whole health' philosophy, recognizing that physical, behavioral, and social factors are deeply intertwined. This commitment is evident in their substantial investments in community initiatives designed to tackle critical social determinants of health, such as food insecurity and improving maternal health outcomes.
The company is actively working to advance health equity, striving to create a future where everyone, irrespective of their background, has a fair chance to achieve optimal health. This focus is crucial in a landscape where disparities in access and quality of care persist.
For instance, in 2024, Elevance Health announced a $100 million commitment over five years to address social drivers of health, with a significant portion allocated to programs that directly impact vulnerable populations and promote equitable access to care.
Consumers are demanding more customized health insurance, with a growing preference for plans that adapt to their specific needs. Elevance Health is responding by using digital tools to create more engaging member experiences and make their services easier to navigate.
This focus on the individual is crucial for improving how people access care and manage their health. For instance, in 2024, Elevance Health reported a significant increase in digital health tool adoption among its members, directly correlating with higher patient satisfaction scores.
Behavioral Health Needs
The demand for mental and behavioral health services is on the rise, with healthcare policies increasingly prioritizing expanded coverage in this critical area. Elevance Health is well-positioned to meet these growing needs through its dedicated behavioral health services and a strong focus on integrated care solutions that holistically address patient well-being. This strategic alignment is crucial as the Centers for Medicare & Medicaid Services (CMS) projected a 6.1% increase in the Medicare Part B physician fee schedule in 2024, which can impact reimbursement for various health services, including behavioral health.
Furthermore, the extension of telehealth flexibilities for certain behavioral and mental health services, a trend accelerated by the COVID-19 pandemic, continues to shape service delivery. This allows for greater accessibility and convenience for individuals seeking support. For instance, the Substance Abuse and Mental Health Services Administration (SAMHSA) reported that in 2023, over 60% of adults with a mental illness received some form of treatment, highlighting the ongoing importance of accessible care.
- Growing Demand: Societal awareness and destigmatization are fueling increased utilization of mental and behavioral health services.
- Policy Support: Healthcare policies are evolving to mandate and incentivize better coverage for behavioral health, reflecting its importance.
- Integrated Care Focus: Elevance Health's strategy emphasizes combining physical and behavioral health, recognizing their interconnectedness.
- Telehealth Expansion: Extended telehealth flexibilities enhance access to crucial mental health support, particularly in underserved areas.
Workforce Shortages and Burnout
Persistent shortages in healthcare professionals, especially nurses and physicians, remain a critical issue across the industry. These staffing gaps directly influence labor expenses and can diminish operational efficiency. For instance, the Association of American Medical Colleges projected a shortage of between 37,800 and 124,000 physicians by 2034 in the US.
The strain on existing staff contributes to elevated burnout rates, which can compromise the quality and availability of patient care. This situation creates a challenging environment for healthcare providers, impacting their ability to meet demand.
As a major health insurance provider, Elevance Health faces indirect consequences from these provider-level workforce challenges. Increased labor costs for healthcare systems may eventually translate to higher reimbursement rates, affecting Elevance's operational costs and potentially influencing premium pricing for its members.
Key impacts include:
- Increased Labor Costs: Higher demand for limited healthcare professionals drives up wages and benefits.
- Reduced Productivity: Fewer staff members mean increased workloads, potentially slowing down service delivery.
- Burnout and Turnover: Overworked staff are more prone to burnout, leading to higher turnover and further exacerbating shortages.
- Impact on Care Access: Shortages can lead to longer wait times and reduced availability of specialized medical services.
Societal shifts toward greater emphasis on mental and behavioral health are a significant driver for Elevance Health. Increased awareness and reduced stigma are leading more individuals to seek care, a trend supported by evolving healthcare policies that advocate for better coverage. Elevance's strategy of integrating physical and behavioral health, alongside expanded telehealth options, directly addresses this growing demand, enhancing accessibility for members.
The company's commitment to addressing social determinants of health, such as food insecurity and maternal health, is a direct response to societal needs and a key component of advancing health equity. For instance, Elevance Health's 2024 pledge of $100 million over five years targets vulnerable populations, aiming to bridge existing care gaps and promote fairer health outcomes.
Consumer demand for personalized healthcare experiences is also shaping Elevance Health's approach. By leveraging digital tools, the company is enhancing member engagement and simplifying access to services, a strategy that has shown positive results, with increased digital tool adoption correlating with higher satisfaction in 2024.
| Sociological Factor | Elevance Health Response/Impact | Supporting Data/Trend |
| Aging Population & Chronic Disease | Increased demand for specialized care and insurance (e.g., Medicare Advantage). | Projections show a substantial senior population in 2024, driving chronic disease management needs. |
| Mental & Behavioral Health Focus | Expansion of behavioral health services and integrated care solutions. | CMS projected a 6.1% increase in Medicare Part B physician fee schedule for 2024; telehealth flexibilities continue to improve access. |
| Health Equity & Social Determinants | Investment in community initiatives targeting food insecurity, maternal health, etc. | $100 million commitment over five years (announced 2024) to address social drivers of health. |
| Consumer Personalization & Digital Engagement | Use of digital tools for tailored experiences and easier navigation. | Significant increase in digital health tool adoption by members in 2024, linked to higher satisfaction. |
Technological factors
Elevance Health is making significant strides in digital transformation, aiming to reshape how members interact with their health services. A key initiative is the ongoing investment in digital solutions designed to both enhance member experiences and optimize internal operations. This focus is evident in the development of advanced digital tools, such as the Sydney Health app, which is central to boosting member engagement through tailored experiences and expanded telehealth capabilities.
The company's strategic objective is to see a substantial rise in digital platform adoption among its member base. For instance, by the end of 2023, Elevance reported that over 30 million members had access to the Sydney Health app, with a notable portion actively using its features. This push towards digital interaction is directly linked to their broader goal of improving overall health outcomes for their covered individuals.
Elevance Health is actively integrating Artificial Intelligence (AI) to transform its operations. The company is leveraging AI for real-time data analysis to improve health outcomes and operational efficiency, with a focus on automating core business processes like claims processing.
This AI deployment is also aimed at providing valuable insights for workforce management. A key consideration in Elevance Health's AI strategy is the paramount importance of protecting consumer privacy throughout these technological advancements.
Telemedicine has cemented its role in healthcare, with regulatory flexibilities extended through 2025, enabling wider adoption. Elevance Health leverages these advancements by integrating virtual and home care models into its offerings, responding to the increasing consumer preference for accessible and adaptable healthcare solutions.
This expansion is supported by data showing significant growth; for instance, the global telemedicine market was valued at approximately $26.9 billion in 2023 and is projected to reach $195.9 billion by 2030, growing at a CAGR of 32.5%. Elevance Health's strategic focus on these virtual services positions it well to capture a share of this expanding market.
However, the long-term landscape of telemedicine is subject to evolving regulatory frameworks. Changes in reimbursement policies and licensing requirements could influence the scope and profitability of these virtual care services, presenting a key technological factor for Elevance Health to monitor and adapt to.
Data Analytics and Predictive Modeling
Elevance Health heavily leverages data analytics and predictive modeling to enhance member health outcomes and manage costs effectively. Their sophisticated use of technologies like machine learning and natural language processing allows for a deep understanding of consumer behavior, enabling highly targeted outreach and personalized care strategies. This data-driven approach is crucial for making informed decisions and driving efficiency within their operations.
The company's investment in these technological capabilities is evident in their pursuit of better health management. For instance, in 2023, Elevance Health reported significant advancements in their digital health solutions, aiming to proactively identify and manage chronic conditions. This focus on predictive analytics helps in anticipating health needs and intervening earlier, which is projected to reduce healthcare expenditures by an estimated 10-15% for specific patient cohorts by 2025.
- Predictive Health Insights: Utilizing AI to forecast disease progression and identify at-risk populations.
- Personalized Member Engagement: Tailoring communication and interventions based on individual health data and preferences.
- Operational Efficiency: Streamlining administrative processes and claims management through advanced analytics.
- Cost Reduction Strategies: Employing data to pinpoint areas of inefficiency and implement targeted cost-saving measures.
Cybersecurity and Data Protection
Cybersecurity is a critical technological factor for Elevance Health, especially as healthcare operations become more digitized. The company must continually invest in robust security measures to safeguard patient data against evolving threats like ransomware and phishing attacks. For instance, the healthcare sector experienced a significant rise in cyberattacks, with reported data breaches affecting millions of individuals in recent years, underscoring the urgency for advanced protection.
Elevance Health's commitment to data protection involves stringent protocols and regular audits to ensure compliance with regulations such as HIPAA. This focus on security not only protects sensitive health information but also builds trust with consumers and healthcare providers. The company's proactive approach includes advanced encryption, multi-factor authentication, and employee training to mitigate risks, aiming for transparency and accountability in its reporting to regulatory bodies.
- Increased reliance on digital health platforms necessitates advanced cybersecurity infrastructure.
- Ransomware and data breaches pose significant threats to patient data confidentiality and operational continuity.
- Elevance Health invests in robust data protection measures to comply with regulations like HIPAA.
- Transparency in reporting security incidents reinforces regulatory compliance and stakeholder trust.
Elevance Health is aggressively expanding its digital footprint, with the Sydney Health app serving as a cornerstone for member engagement, reporting over 30 million members with access by the close of 2023. This digital push is amplified by a strategic integration of Artificial Intelligence (AI) to streamline operations, particularly in claims processing and workforce management, aiming for enhanced efficiency and improved health outcomes.
The company is also capitalizing on the growth of telemedicine, a sector valued at approximately $26.9 billion in 2023 and projected to reach $195.9 billion by 2030, with a CAGR of 32.5%. This expansion into virtual and home care models aligns with consumer preferences and regulatory flexibility extended through 2025, though evolving reimbursement policies remain a key factor to monitor.
Data analytics and predictive modeling are central to Elevance Health's strategy, utilizing machine learning and natural language processing to personalize care and manage costs. In 2023, the company reported advancements in digital health solutions to proactively manage chronic conditions, with projections indicating potential healthcare expenditure reductions of 10-15% for specific patient groups by 2025.
Cybersecurity remains a paramount concern, with the healthcare sector facing increasing threats; Elevance Health invests heavily in robust measures, including advanced encryption and multi-factor authentication, to protect sensitive patient data and ensure compliance with regulations like HIPAA, thereby fostering stakeholder trust.
Legal factors
Elevance Health navigates a complex legal landscape, notably the Health Insurance Portability and Accountability Act (HIPAA). The period of 2024-2025 sees significant proposed updates to HIPAA, aiming to bolster patient data security and privacy. These revisions are crucial for maintaining trust and operational integrity.
Beyond federal mandates, Elevance Health must also contend with a growing number of state-specific laws governing consumer health data. For instance, California's Consumer Privacy Act (CCPA) and its subsequent amendments continue to shape data handling practices. Staying ahead of these evolving regulatory requirements is paramount for compliance and avoiding potential penalties.
The legal landscape for telehealth is actively evolving, with current flexibilities, such as those allowing for a wider range of originating sites, extended through December 31, 2025. This means Elevance Health must remain agile, preparing for potential permanent changes to these regulations.
Key areas demanding close attention for Elevance Health include the finalization of originating site requirements and the ongoing reimbursement policies for audio-only telehealth services. Navigating these shifts is crucial for maintaining compliant operations and ensuring continued access to care for their members.
Elevance Health's significant exposure to government-sponsored health plans like Medicare and Medicaid means it must navigate a constantly shifting regulatory landscape. Changes in reimbursement rates, eligibility criteria, and new requirements for beneficiaries, such as work mandates for Medicaid, directly influence membership numbers and overall financial results. For instance, a shift in Medicare Advantage payment rates, which are adjusted annually, can have a material impact on Elevance's profitability for that segment.
Antitrust and Market Conduct Scrutiny
Elevance Health, as a major player in the health insurance sector, faces significant antitrust and market conduct scrutiny. Regulators keep a close eye on its business practices to ensure fair competition and prevent monopolistic behavior. This oversight is crucial in a market where market share can significantly impact consumer choice and pricing.
The company must navigate a complex web of antitrust laws, which govern everything from pricing strategies to mergers and acquisitions. For instance, in 2024, the Federal Trade Commission (FTC) continued its aggressive stance on healthcare consolidation, reviewing numerous proposed mergers. Elevance Health needs to demonstrate that its actions do not harm competition, particularly in its key markets.
Compliance with these regulations is paramount. Elevance Health's strategy for growth, including potential acquisitions or strategic partnerships, must be carefully vetted to avoid violating antitrust statutes. Failure to comply can result in hefty fines, divestitures, and damage to the company's reputation.
- Market Share Monitoring: Elevance Health's substantial market share in several states necessitates ongoing monitoring by antitrust authorities.
- Acquisition Reviews: Any proposed mergers or acquisitions by Elevance Health are subject to rigorous review by bodies like the FTC and Department of Justice.
- Partnership Scrutiny: Collaborations and exclusive agreements with providers or other entities are examined for potential anti-competitive effects.
- Pricing Practices: Regulators assess Elevance Health's pricing models to ensure they are not predatory or indicative of market manipulation.
Litigation and Compliance Risks
Elevance Health navigates a landscape fraught with litigation and compliance risks, including potential government investigations, audits, and reviews concerning its operational practices and claims processing. The company's commitment to its Code of Conduct, which stresses meticulous record-keeping and strict adherence to legal mandates, serves as a primary strategy to mitigate these exposures. For instance, in 2023, the healthcare sector saw increased scrutiny on billing practices, with fines levied against various entities for non-compliance, underscoring the importance of Elevance's preventative measures.
These legal challenges can significantly impact financial performance and reputation. Elevance's proactive approach aims to preempt costly penalties and operational disruptions. The company's robust compliance programs are designed to ensure alignment with evolving regulatory frameworks, such as those governed by the Centers for Medicare & Medicaid Services (CMS), which directly influence revenue streams and operational procedures.
Elevance Health operates under stringent healthcare regulations, including those from the Centers for Medicare & Medicaid Services (CMS). For 2024, CMS finalized Medicare Advantage and Part D payment rates, impacting revenue projections. The company also faces state-specific insurance laws and consumer protection statutes, such as those in New York, which can influence plan offerings and marketing practices.
Antitrust scrutiny remains a significant legal factor. In 2024, the Federal Trade Commission (FTC) continued its focus on healthcare market concentration. Elevance Health's market share in key regions, like Ohio where it holds a substantial portion of the individual market, draws regulatory attention regarding potential anti-competitive practices.
The evolving legal framework for telehealth services, with flexibilities extended through December 31, 2025, requires Elevance Health to adapt its service delivery models. Compliance with data privacy laws, including updated HIPAA provisions proposed for 2024-2025, is critical to protect member information and avoid legal repercussions.
| Legal Area | Key Regulation/Factor | Impact on Elevance Health (2024-2025) | Example/Data Point |
|---|---|---|---|
| Data Privacy | HIPAA Updates | Enhanced data security requirements, potential compliance costs. | Proposed rule aims to strengthen patient data protection. |
| Antitrust | FTC Enforcement | Scrutiny on market share and potential mergers. | FTC's active review of healthcare consolidations in 2024. |
| Government Programs | CMS Payment Rules | Direct impact on revenue from Medicare Advantage and Medicaid. | Annual adjustments to Medicare Advantage payment rates. |
| Telehealth | Regulatory Flexibilities | Need for adaptation to evolving telehealth service delivery and reimbursement. | Flexibilities extended through December 31, 2025. |
Environmental factors
Elevance Health acknowledges that environmental shifts, including ecological disruptions and altered weather, directly impact health. These factors influence physical, behavioral, and social health determinants, creating a complex web of challenges for member well-being.
The worsening of chronic conditions like asthma and cardiovascular issues is a direct consequence of these environmental changes. For instance, increased air pollution linked to climate change can exacerbate respiratory ailments, leading to higher healthcare utilization and costs for Elevance Health members.
The World Health Organization estimates that between 2030 and 2050, climate change could cause approximately 250,000 additional deaths per year from malnutrition, malaria, diarrhea, and heat stress alone. This underscores the significant financial and operational implications for health insurers like Elevance Health.
Elevance Health is actively pursuing decarbonization within the healthcare sector, aiming for net-zero emissions across scope 1, 2, and 3. This commitment is demonstrated by their achievement of sourcing 100% renewable electricity for operations ahead of schedule, highlighting a proactive approach to environmental responsibility.
Elevance Health is actively working with its key suppliers to encourage them to adopt science-based targets for reducing greenhouse gas emissions. This initiative is a crucial part of their broader environmental strategy, extending their commitment to sustainability beyond their own facilities.
By pushing for supply chain sustainability, Elevance Health aims to reduce its indirect environmental impact. For instance, in 2023, the company reported a Scope 3 emissions intensity of 0.15 metric tons of CO2e per $1 million in revenue, highlighting the significance of supplier engagement in achieving overall carbon reduction goals.
Community and Climate Resiliency
Elevance Health actively champions community and climate resilience, integrating these principles into its core health strategies and business operations. This commitment extends to partnerships aimed at bolstering local preparedness and recovery efforts.
The Elevance Health Foundation plays a crucial role, offering financial aid and collaborating with disaster relief organizations. For instance, in 2023, the foundation provided over $5 million in grants to support communities impacted by natural disasters, underscoring a dedication to environmental and social well-being.
- Disaster Relief Funding: In 2023, Elevance Health Foundation allocated more than $5 million to disaster relief initiatives.
- Community Partnerships: The company partners with various non-profits and governmental agencies to enhance local resilience.
- Climate-Conscious Operations: Elevance Health is implementing strategies to reduce its carbon footprint across its facilities, aiming for a 20% reduction by 2027.
Environmental, Social, and Governance (ESG) Reporting
Elevance Health demonstrates a robust commitment to Environmental, Social, and Governance (ESG) principles, evidenced by its consistently high ratings from independent assessment agencies. The company actively publishes detailed impact reports that quantify its contributions to whole-health solutions, fostering innovation, and advancing sustainability initiatives. This dedication to transparent ESG reporting underscores Elevance Health's accountability to its stakeholders, including investors and regulatory bodies, concerning its environmental stewardship and broader corporate responsibility.
In 2023, Elevance Health reported a significant reduction in its Scope 1 and Scope 2 greenhouse gas emissions, achieving a 15% decrease compared to its 2020 baseline. The company also achieved a 90% waste diversion rate across its major facilities by the end of 2024, a key metric in its sustainability goals.
- ESG Ratings: Consistently high scores from agencies like MSCI and Sustainalytics, reflecting strong performance in environmental management and social impact.
- Impact Reporting: Publication of annual reports detailing measurable progress on sustainability targets and community well-being initiatives.
- Environmental Metrics: Focused efforts on reducing carbon footprint and improving waste management, with specific targets set for 2025.
- Accountability: Commitment to transparent disclosure ensures stakeholders are informed about the company's environmental practices and progress.
Environmental factors significantly influence Elevance Health's operations and member well-being, with climate change exacerbating chronic conditions and increasing healthcare utilization.
The company is actively pursuing decarbonization, aiming for net-zero emissions and achieving 100% renewable electricity sourcing for its operations ahead of schedule.
Elevance Health also focuses on supply chain sustainability and community resilience, with its foundation providing substantial disaster relief funding, such as over $5 million in 2023.
By the end of 2024, Elevance Health achieved a 90% waste diversion rate across its major facilities, demonstrating a commitment to environmental metrics.
| Environmental Initiative | 2023/2024 Data | Target/Goal |
|---|---|---|
| Scope 1 & 2 GHG Emissions Reduction | 15% reduction vs. 2020 baseline | Ongoing reduction |
| Renewable Electricity Sourcing | 100% achieved | Ahead of schedule |
| Waste Diversion Rate | 90% achieved (by end of 2024) | High diversion rate |
| Disaster Relief Funding (Elevance Health Foundation) | Over $5 million | Community support |
| Scope 3 Emissions Intensity | 0.15 metric tons CO2e per $1 million revenue | Reduction through supplier engagement |
PESTLE Analysis Data Sources
Our PESTLE analysis for Elevance Health is informed by a comprehensive review of publicly available data, including government health policy updates, economic indicators from organizations like the Bureau of Labor Statistics and the Congressional Budget Office, and industry-specific reports from reputable healthcare research firms. We also incorporate insights from relevant legislative changes and technological advancements impacting the healthcare sector.
