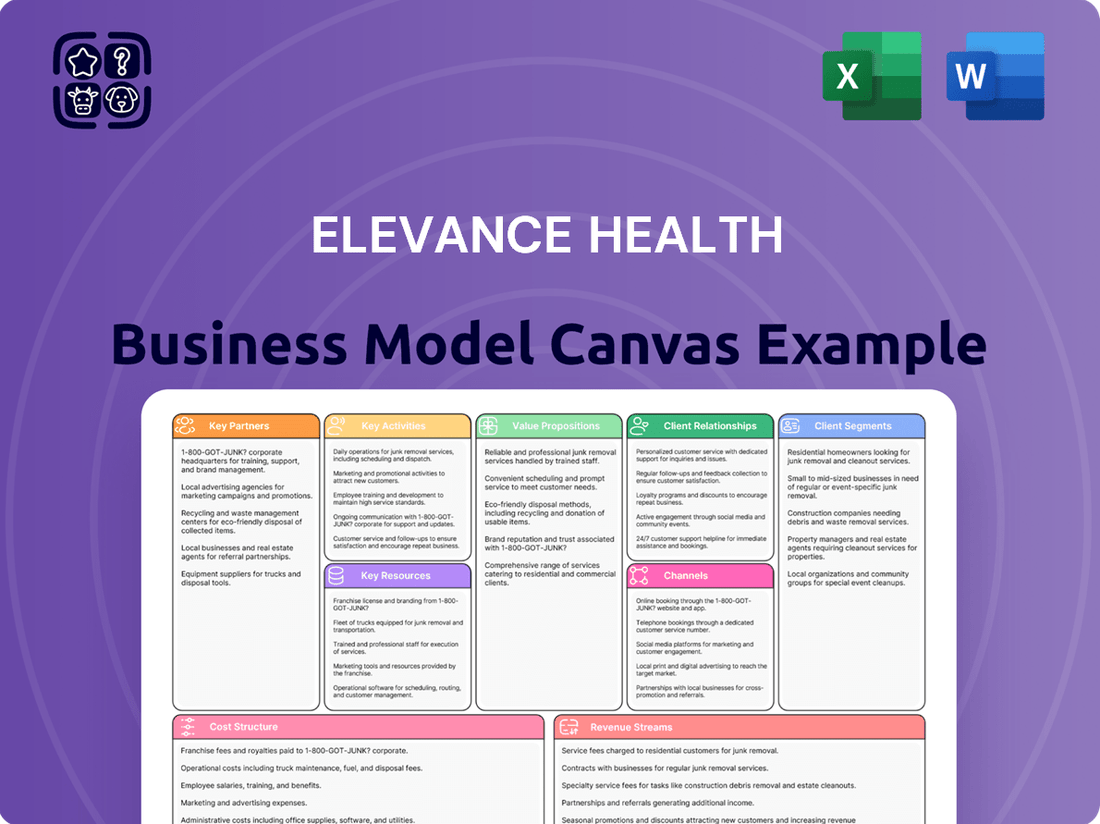
Elevance Health Business Model Canvas
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
Elevance Health Bundle
Unlock the core strategies behind Elevance Health's expansive healthcare ecosystem. This Business Model Canvas dissects their approach to value creation, customer relationships, and revenue streams, offering a clear view of their operational excellence. Discover how they manage key resources and partnerships to deliver integrated health solutions.
Partnerships
Elevance Health cultivates deep relationships with hospitals, clinics, and individual practitioners to create robust healthcare networks. These partnerships are fundamental to offering coordinated care and managing patient well-being effectively. In 2023, Elevance Health reported that its provider network served over 120 million people, underscoring the scale of these collaborations in delivering accessible medical services.
Elevance Health's CarelonRx segment actively collaborates with Pharmacy Benefit Managers (PBMs) and pharmaceutical companies. These crucial alliances enable the provision of comprehensive pharmacy services, encompassing claims processing, formulary development, and maintaining extensive prescription drug databases.
These partnerships are fundamental to ensuring members have affordable access to necessary medications and for effectively controlling overall pharmacy expenditures. For instance, in 2023, CarelonRx managed over 2.1 billion prescription claims, highlighting the scale and importance of these relationships in managing drug costs and access for Elevance Health's vast membership base.
Elevance Health actively partners with community-based organizations and social support services to tackle critical social determinants of health. These collaborations are vital for addressing issues like food insecurity, housing instability, and behavioral health challenges, which significantly impact member well-being. For instance, in 2024, Elevance expanded its housing support programs, aiming to reduce homelessness among its members by 15% by the end of the year.
These partnerships extend beyond traditional healthcare, offering members comprehensive support that enhances their overall health outcomes. By integrating social services with medical care, Elevance Health fosters a more holistic approach to member wellness. In 2023, Elevance reported that members engaged with these community programs showed a 20% lower rate of hospital readmissions compared to those not participating.
Technology and Digital Health Solution Providers
Elevance Health actively partners with technology and digital health solution providers to weave advanced capabilities into its service offerings. These collaborations are crucial for developing and integrating cutting-edge digital health solutions, such as sophisticated telehealth platforms and AI-driven tools designed to streamline claims processing. For instance, the Sydney Health app leverages these partnerships to deliver personalized care recommendations directly to members.
These strategic alliances are instrumental in fostering innovation across Elevance Health’s operations. They enable the company to enhance member engagement through more intuitive and accessible digital touchpoints. Furthermore, these partnerships significantly contribute to improving operational efficiency by automating processes and providing data-driven insights.
- Digital Health Integration: Collaborations focus on integrating telehealth, AI for claims, and personalized care apps like Sydney Health.
- Innovation Driver: Partnerships fuel the development of new digital health tools and services.
- Member Engagement: Technology partners help create more interactive and personalized experiences for Elevance Health members.
- Operational Efficiency: These alliances aim to streamline administrative tasks and improve overall business processes.
Employers and Broker Networks
Elevance Health collaborates with employers of all sizes, from small businesses to large corporations, to provide comprehensive group health insurance and employee benefits. This partnership allows them to offer tailored solutions that meet diverse workforce needs.
Crucially, Elevance Health relies on extensive broker networks to distribute its wide array of health plans. These networks are instrumental in reaching a broad spectrum of potential members within the commercial insurance markets, driving membership growth and market penetration.
For instance, in 2024, Elevance Health continued to leverage these relationships to expand its commercial membership, which forms a significant portion of its overall business. The strength of these employer and broker relationships directly impacts the company's ability to secure and retain customers.
- Employer Partnerships: Elevance Health offers customized group health insurance and benefits packages to businesses of all sizes, fostering long-term relationships.
- Broker Network Vitality: The company's distribution strategy heavily relies on a robust network of insurance brokers to market and sell its diverse health plans.
- Market Reach: These partnerships are key to accessing and serving a wide customer base across various commercial markets.
Elevance Health's key partnerships are diverse, spanning healthcare providers, pharmaceutical entities, community organizations, technology firms, employers, and brokers. These collaborations are essential for delivering coordinated care, managing costs, addressing social determinants of health, driving innovation, and expanding market reach.
| Partner Type | Purpose | Impact/Example |
|---|---|---|
| Healthcare Providers | Network development, coordinated care | Serving over 120 million people in 2023 |
| PBMs & Pharma Companies | Pharmacy services, formulary management | Managed over 2.1 billion prescription claims in 2023 |
| Community Organizations | Addressing social determinants of health | Expanded housing support in 2024 |
| Technology Providers | Digital health solutions, operational efficiency | Sydney Health app integration |
| Employers & Brokers | Distribution, membership growth | Expanding commercial membership in 2024 |
What is included in the product
This Elevance Health Business Model Canvas provides a comprehensive overview of their strategy, detailing customer segments, value propositions, and key partnerships. It offers insights into their revenue streams and cost structure, reflecting their operational approach to healthcare delivery.
Elevance Health's Business Model Canvas acts as a pain point reliever by providing a clear, one-page snapshot of their complex healthcare ecosystem, simplifying understanding and strategic alignment.
Activities
Elevance Health's key activities center on the meticulous management and administration of a diverse array of health plans. This includes not only traditional options like HMOs and PPOs but also government-sponsored programs such as Medicare and Medicaid, demonstrating a broad reach across the healthcare landscape.
Underwriting, claims processing, and policy administration form the backbone of these operations. For instance, in 2023, Elevance Health processed billions of claims, a testament to the scale of their administrative capabilities and their commitment to efficient service delivery for millions of members.
Ensuring strict adherence to regulatory compliance is paramount in this domain. Elevance Health navigates complex legal frameworks to maintain the integrity and legality of its plan offerings, safeguarding both the company and its beneficiaries. Their focus on compliance is critical for maintaining trust and operational continuity.
Elevance Health actively manages member health through comprehensive care coordination, focusing on areas like behavioral health and chronic conditions. This approach aims to improve overall health outcomes by ensuring seamless transitions and integrated care across various providers and settings.
In 2024, Elevance Health continued to emphasize these care management activities. For instance, their integrated approach to behavioral health saw significant investment, aiming to address the growing demand for mental health services. This focus is critical as studies in 2024 highlighted the direct correlation between accessible behavioral health support and better management of chronic physical ailments.
Elevance Health's CarelonRx segment is central to its pharmacy services delivery, encompassing operations like home delivery and specialty pharmacies. This segment ensures members have access to essential medications through careful formulary management, a critical component of their integrated health solutions.
In 2024, CarelonRx continued to focus on enhancing member access and affordability. The company reported significant growth in its pharmacy benefit management (PBM) business, with total PBM revenue reaching $38.6 billion in the first quarter of 2024, a 10.4% increase year-over-year, highlighting the scale of its pharmacy operations.
Digital Health Innovation and Development
Elevance Health's commitment to digital health innovation is a cornerstone of its strategy. A primary key activity involves the continuous investment in and development of cutting-edge digital health solutions. This includes enhancing platforms like the Sydney Health app and leveraging artificial intelligence for more sophisticated tools.
These digital advancements are designed to streamline the entire healthcare journey for consumers. By simplifying access and providing personalized insights, Elevance aims to empower individuals in managing their health more effectively. The focus is on creating a more intuitive and user-friendly experience, ultimately improving overall care delivery through technology.
In 2023, Elevance Health reported significant growth in its digital engagement, with millions of members actively using its digital tools. The Sydney Health app, for instance, saw a substantial increase in daily active users, reflecting a growing reliance on digital platforms for health management. This digital push is directly tied to Elevance's goal of improving health outcomes and reducing healthcare costs through accessible, technology-driven solutions.
- Continuous Investment: Ongoing funding for research and development of new digital health technologies.
- Platform Enhancement: Regular updates and feature additions to existing digital tools like the Sydney Health app.
- AI Integration: Development and deployment of AI-powered solutions for personalized health insights and improved diagnostics.
- User Experience Focus: Prioritizing ease of use and accessibility to encourage widespread adoption by members.
Provider Network Development and Relationship Management
Elevance Health focuses on building and nurturing a vast network of healthcare providers, including hospitals, physicians, and specialized facilities. This proactive approach ensures members have access to a wide range of quality care options.
Strong relationships are key to this process. Elevance Health actively manages these partnerships to promote collaboration and enhance the overall patient experience.
- Provider Network Growth: In 2024, Elevance Health continued to expand its provider network, aiming for greater geographic coverage and specialty access for its members.
- Relationship Management Initiatives: The company invested in programs designed to improve communication and satisfaction among its contracted providers, recognizing their critical role in delivering value-based care.
- Quality and Access Metrics: Efforts are consistently directed towards ensuring that the provider network meets high standards for quality of care and accessibility, directly impacting member health outcomes.
Elevance Health's key activities are multifaceted, encompassing the administration of health plans, processing claims, and ensuring regulatory compliance. They also focus on proactive member health management, particularly in behavioral health and chronic conditions.
A significant activity involves managing the CarelonRx segment for pharmacy services, including home delivery and specialty pharmacies, with a strong emphasis on PBM growth. Furthermore, Elevance Health invests heavily in digital health innovation, enhancing platforms like the Sydney Health app to improve member experience and health outcomes.
Building and maintaining a robust network of healthcare providers is another crucial activity, ensuring members have access to quality care through strong provider relationships and network expansion initiatives.
| Key Activity | Description | 2024 Data/Focus |
|---|---|---|
| Health Plan Administration | Managing diverse health plans (HMO, PPO, Medicare, Medicaid) and processing claims. | Continued efficient claims processing for millions of members. |
| Member Health Management | Care coordination for behavioral health and chronic conditions. | Increased investment in integrated behavioral health solutions. |
| Pharmacy Services (CarelonRx) | Operating PBM, home delivery, and specialty pharmacies. | Focus on member access and affordability; PBM revenue grew 10.4% YoY in Q1 2024. |
| Digital Health Innovation | Developing and enhancing digital tools like Sydney Health app. | Continued investment in AI for personalized health insights. |
| Provider Network Management | Building and managing relationships with healthcare providers. | Expansion of provider network for greater geographic coverage and specialty access. |
Preview Before You Purchase
Business Model Canvas
The Elevance Health Business Model Canvas you are previewing is the exact document you will receive upon purchase. This isn't a sample or mockup; it's a direct representation of the comprehensive analysis you'll gain. You'll get full access to this professionally structured and detailed canvas, ready for immediate use and strategic planning.
Resources
Elevance Health's extensive provider network, encompassing a wide array of hospitals, physicians, and specialists, is a cornerstone of its business model. This vast network, cultivated through strategic contracting, directly translates into broad access to medical services for its over 100 million members across various plans. In 2024, maintaining and expanding these relationships is paramount to delivering on the promise of comprehensive and convenient care.
Elevance Health's proprietary technology, including the Sydney Health app and its Health OS platform, is a cornerstone of its business model. These advanced systems enable the company to deliver personalized health recommendations and streamline member engagement.
The company's robust data analytics capabilities are critical for optimizing operations, such as processing claims efficiently. In 2023, Elevance Health reported a significant increase in digital engagement, with millions of members actively using its platforms, highlighting the growing importance of these technological assets.
Elevance Health’s human capital, particularly its clinical expertise, is a cornerstone of its business model. This includes a vast network of physicians, nurses, care managers, and allied health professionals whose deep understanding of medicine and patient care is crucial for delivering high-quality services. In 2024, Elevance Health continued to invest in its workforce, recognizing that skilled professionals are essential for managing chronic conditions, coordinating care, and driving positive health outcomes for its members.
The company’s operational knowledge, embedded within its technical specialists and administrative staff, further enhances its ability to manage complex healthcare needs efficiently. This expertise allows Elevance Health to navigate regulatory landscapes, implement innovative care models, and leverage technology to improve member engagement and provider collaboration. The commitment to continuous training and development ensures this workforce remains at the forefront of healthcare advancements.
Brand Recognition and Market Presence
Elevance Health leverages its robust brand recognition, notably through its Blue Cross Blue Shield (BCBS) licenses in numerous states, to solidify its significant market presence across the United States. This established brand equity and substantial scale are foundational to its ability to attract and retain both members and strategic partners.
The company's market penetration is substantial. For instance, in 2023, Elevance Health served approximately 115 million people, a testament to its widespread reach and the trust consumers place in its brands.
- Brand Equity: Strong association with the trusted Blue Cross Blue Shield name in key markets.
- Market Share: Significant presence in multiple U.S. states, enabling economies of scale.
- Member Acquisition: Brand strength directly contributes to attracting and retaining a large member base.
- Partnership Attraction: A recognized and scaled brand is more appealing to potential healthcare providers and employers.
Financial Capital and Reserves
Elevance Health maintains substantial financial capital and reserves, a critical component for managing its operations. These reserves are essential for covering the significant volume of medical claims it processes, ensuring timely payments to healthcare providers and members.
This financial strength also fuels strategic investments. In 2024, Elevance Health continued to allocate capital towards enhancing its digital capabilities and data analytics, aiming to improve member experience and operational efficiency. Furthermore, robust reserves provide the necessary backing for potential strategic acquisitions, allowing the company to expand its market reach and service offerings in the dynamic healthcare landscape.
- Financial Stability: Substantial capital ensures Elevance Health can meet its obligations, including medical claims, and navigate economic fluctuations.
- Investment Capacity: Reserves fund investments in technology, such as artificial intelligence for claims processing and personalized member engagement platforms.
- Strategic Growth: Financial reserves enable the pursuit of mergers and acquisitions, as seen in past strategic moves to broaden healthcare solutions.
Elevance Health's key resources are multifaceted, encompassing its vast provider network, proprietary technology platforms like Sydney Health, significant brand equity primarily through its Blue Cross Blue Shield licenses, substantial financial capital, and its skilled human capital. These elements collectively enable the company to deliver comprehensive healthcare services to millions of Americans.
In 2023, Elevance Health served approximately 115 million people, underscoring the reach of its provider network and brand strength. The company's investment in digital engagement, with millions of members actively using its platforms, highlights the growing importance of its technology resources. Financial reserves in 2024 continued to support investments in digital capabilities and data analytics.
| Key Resource | Description | 2023/2024 Data Point |
| Provider Network | Extensive network of hospitals, physicians, and specialists | Cultivated through strategic contracting for broad access |
| Proprietary Technology | Sydney Health app, Health OS platform | Millions of members actively using platforms in 2023 |
| Brand Equity | Blue Cross Blue Shield licenses in numerous states | Significant market presence across the U.S. |
| Financial Capital | Substantial reserves for operations and investments | Continued allocation towards digital capabilities and data analytics in 2024 |
| Human Capital | Clinical expertise, care managers, administrative staff | Investment in workforce for managing chronic conditions and driving health outcomes |
Value Propositions
Elevance Health's commitment to providing comprehensive and diverse health plans is a cornerstone of its value proposition. They offer a broad spectrum of options, including Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), Medicare Advantage, Medicaid, and various employer-sponsored plans. This extensive portfolio ensures that individuals and families with different health requirements and financial capacities can find suitable coverage.
In 2024, Elevance Health continued to demonstrate this commitment by serving millions of members across its various plans. For instance, their Medicare Advantage plans alone served a significant portion of the eligible population, reflecting the demand for tailored government-sponsored health solutions. This wide reach underscores their ability to adapt to diverse market needs and regulatory environments, offering robust health solutions to a broad customer base.
Elevance Health champions a holistic view of health, recognizing that physical, mental, and social well-being are interconnected. They integrate these dimensions through comprehensive care management programs and strategic pharmacy services.
In 2024, Elevance Health continued to expand its community partnerships, a key element in addressing social determinants of health. These collaborations are designed to directly impact patient outcomes by providing access to resources that support overall wellness, moving beyond traditional medical treatment.
Elevance Health prioritizes making healthcare accessible by providing cost-effective insurance plans. For instance, in 2023, the company reported that its focus on value-based care initiatives helped manage medical expenses, contributing to a more predictable cost structure for its members and employers.
The company actively manages medical expenses through disciplined strategies, aiming to reduce the overall financial burden on its customers. This commitment to cost control is a cornerstone of their offering, ensuring that members benefit from lower out-of-pocket expenses.
A key element of Elevance Health's affordability strategy is its emphasis on preventive care. By encouraging proactive health management, they aim to reduce the incidence of costly chronic conditions, ultimately lowering healthcare spending for individuals and businesses alike.
Simplified Healthcare Experience through Digital Solutions
Elevance Health simplifies healthcare by integrating digital tools like the Sydney Health app. This platform uses AI to offer members easy access to their health data, personalized guidance, and smoother interactions with the healthcare system.
The company's digital strategy focuses on making healthcare more user-friendly and accessible. By streamlining processes and providing tailored support, Elevance Health aims to improve member engagement and health outcomes.
- Digital Engagement: The Sydney Health app serves as a central hub for members, offering features like finding care, managing prescriptions, and accessing wellness programs.
- AI-Powered Personalization: Artificial intelligence is employed to deliver personalized health insights and recommendations, guiding members toward better health decisions.
- Streamlined Interactions: Technology is used to reduce administrative burdens and simplify communication, making it easier for members to navigate their healthcare journey.
- Focus on Member Experience: The core value proposition is to create a more intuitive and supportive healthcare experience, moving away from traditional, often complex, systems.
Extensive Access to Quality Care
Elevance Health leverages its substantial network to offer members broad access to quality healthcare. This extensive provider network is a core value proposition, ensuring convenient and varied choices for medical services.
In 2024, Elevance Health continued to focus on expanding its provider relationships. This commitment translates into tangible benefits for members, offering a wide selection of doctors, specialists, and facilities.
- Extensive Provider Network: Elevance Health boasts a large and diverse network of healthcare professionals and facilities across its service areas.
- Quality of Care: The company prioritizes partnerships with providers who meet high standards for medical expertise and patient outcomes.
- Member Convenience: This broad access reduces wait times and travel burdens, making it easier for members to receive timely and appropriate care.
- Choice and Flexibility: Members have the freedom to select providers that best suit their individual health needs and preferences.
Elevance Health's value proposition centers on providing a wide array of health plan options, from HMOs to Medicare Advantage, catering to diverse needs and budgets.
They champion a holistic approach to health, integrating mental and social well-being into their care management programs, as evidenced by their 2024 community partnerships focused on social determinants of health.
Affordability is key, achieved through cost-effective plans and a strong emphasis on preventive care, which helped manage medical expenses in 2023.
Digital tools like the Sydney Health app enhance member experience by offering personalized guidance and simplifying healthcare navigation.
| Value Proposition Aspect | Description | 2024 Relevance/Data Point |
|---|---|---|
| Comprehensive Health Plans | Broad spectrum of plan types (HMO, PPO, Medicare Advantage, Medicaid) | Serves millions of members across diverse plans, including a significant portion of eligible Medicare Advantage beneficiaries. |
| Holistic Health Approach | Integration of physical, mental, and social well-being | Expanded community partnerships in 2024 to address social determinants of health and improve overall wellness. |
| Affordability and Cost Management | Cost-effective plans and focus on preventive care | Value-based care initiatives in 2023 contributed to managing medical expenses and predictable cost structures for members. |
| Digital Engagement and Simplification | AI-powered tools like Sydney Health app | Continual enhancement of the Sydney Health app for personalized insights and streamlined member interactions. |
| Extensive Provider Network | Broad access to quality healthcare providers | Ongoing focus in 2024 to expand provider relationships, ensuring member convenience and choice. |
Customer Relationships
Elevance Health champions personalized member support through dedicated advocacy, acting as a single point of contact. This strategy helps members navigate benefits and manage chronic conditions, building trust and loyalty.
In 2024, Elevance Health continued to emphasize these relationships, with a significant portion of its member engagement efforts focused on proactive outreach and personalized guidance. This commitment aims to improve health outcomes and member satisfaction.
Elevance Health heavily leverages digital platforms, including its website and mobile app, to foster strong customer relationships. These digital tools are central to empowering members with self-service capabilities, allowing them to easily manage their health plans, access vital health information, and even connect with healthcare providers. This digital-first approach not only boosts convenience but also puts control directly into the hands of their members.
Elevance Health fosters strong customer relationships through deep community engagement and dedicated health equity initiatives. In 2024, the company continued to invest in programs aimed at addressing social determinants of health, such as access to healthy food and safe housing, directly impacting the well-being of vulnerable populations.
These efforts go beyond traditional healthcare, reflecting a commitment to broader societal well-being and building trust by actively supporting community health. This proactive approach helps create lasting connections with members and the communities they serve.
Employer Relationship Management
Elevance Health cultivates robust employer relationships by offering customized group health insurance and benefits packages. This approach centers on deeply understanding each employer's unique requirements and delivering comprehensive support to their employees.
The company's strategy emphasizes proactive engagement and partnership. In 2024, Elevance Health reported serving over 120 million members, a testament to the trust built with employer groups through consistent service and adaptable solutions.
- Tailored Benefits: Providing group health insurance plans specifically designed to meet the diverse needs of employer workforces.
- Comprehensive Support: Offering dedicated resources and assistance to employers and their employees for seamless benefit administration and utilization.
- Long-Term Partnerships: Focusing on building enduring relationships through consistent value delivery and responsiveness to evolving employer needs.
Provider Collaboration and Support
Elevance Health fosters strong provider partnerships by providing essential tools and resources designed to enhance patient safety and clinical outcomes. This collaborative model ensures providers are actively engaged in achieving shared goals for high-quality care delivery.
- Provider Support: Offering digital platforms and analytics to streamline workflows and improve patient management.
- Value-Based Care: Implementing payment models that reward providers for quality and efficiency, aligning incentives.
- Outcome Focus: Collaborating on initiatives that directly improve patient health and reduce adverse events.
- 2024 Data: Elevance Health reported a significant increase in providers participating in value-based care arrangements, indicating a growing alignment with quality-focused partnerships.
Elevance Health cultivates member loyalty through personalized advocacy, digital empowerment, and community-focused health equity initiatives. These strategies, emphasized in 2024, aim to improve health outcomes and build lasting trust by addressing social determinants of health. By offering tailored benefits and comprehensive support, Elevance Health also builds robust employer relationships, serving over 120 million members in 2024.
| Relationship Type | Key Strategies | 2024 Impact/Focus |
|---|---|---|
| Member Relationships | Personalized advocacy, digital platforms (app/website), community engagement, health equity programs | Improved health outcomes, increased member satisfaction, addressing social determinants of health |
| Employer Relationships | Customized group health insurance, dedicated support, long-term partnership focus | Serving over 120 million members, consistent service delivery |
| Provider Partnerships | Essential tools/resources, value-based care models, outcome-focused collaboration | Increased provider participation in value-based care, improved patient safety and clinical outcomes |
Channels
Elevance Health leverages direct sales teams to connect with potential members, offering personalized guidance on plan selection. These teams are vital for engaging individuals and small businesses directly, explaining complex benefits and enrollment processes.
Furthermore, a robust network of independent brokers and agents acts as a critical distribution channel. In 2024, these broker relationships were instrumental in reaching employers of all sizes, facilitating the sale of Elevance Health's diverse portfolio of health insurance products.
Elevance Health leverages digital channels, including its website and the Sydney Health mobile app, as key touchpoints for members. These platforms facilitate plan selection, benefit management, and access to health resources. In 2024, the company continued to invest in these digital assets to improve member experience and engagement, with Sydney Health offering features like personalized health insights and virtual care options.
Elevance Health leverages employer benefit programs as a primary channel to reach its employer customer segment. This strategic approach allows businesses to integrate Elevance Health's comprehensive health plans directly into their employee benefits packages, simplifying the process for both employers and their workforce.
Through these established channels, companies can effectively offer health coverage as a key component of their total compensation, enhancing employee satisfaction and retention. In 2024, employer-sponsored health insurance remained a cornerstone of healthcare access for millions of Americans, with Elevance Health playing a significant role in this ecosystem.
Government Program Administrations
Elevance Health effectively utilizes its robust administrative infrastructure to manage and deliver services for government-sponsored healthcare programs, notably Medicare and Medicaid. These programs are crucial conduits for engaging with distinct demographic segments, encompassing the elderly, individuals with limited financial resources, and those with disabilities.
These government programs represent a substantial portion of Elevance Health's revenue. In 2023, for instance, government business accounted for approximately 67% of Elevance Health's total revenue, underscoring their importance as a channel. This strategic focus allows Elevance Health to serve a broad and diverse patient base.
- Medicare: Serving over 65 million beneficiaries in 2024, Medicare is a primary channel for reaching senior populations.
- Medicaid: Providing coverage to over 90 million Americans in 2024, Medicaid is key for accessing low-income individuals and families.
- Dual Eligibles: Elevance Health also serves individuals eligible for both Medicare and Medicaid, a complex but vital demographic.
- Government Contracts: The company actively pursues and manages contracts with federal and state agencies to administer these programs.
Healthcare Provider Referrals and Partnerships
Healthcare providers within Elevance Health's network are a crucial channel for member acquisition, leveraging referrals to expand their reach. These partnerships are vital for fostering integrated care delivery, a key driver for increasing enrollment by offering a seamless patient experience.
Elevance Health actively cultivates these provider relationships. For instance, in 2023, Elevance Health reported that approximately 60% of its revenue was derived from its health plan business, with a significant portion of that growth attributed to expanding provider networks and member engagement strategies, which include referral programs.
- Provider Referrals: Healthcare providers act as a direct channel for acquiring new members through patient recommendations.
- Integrated Care: Strong provider partnerships enable coordinated care, enhancing member satisfaction and retention.
- Enrollment Growth: Effective referral programs and integrated care models contribute directly to higher enrollment numbers.
- Network Expansion: Elevance Health's strategy includes growing its network of providers to capture a larger share of the market through these trusted relationships.
Elevance Health utilizes a multi-faceted channel strategy, including direct sales, independent brokers, digital platforms, employer benefit programs, and government-sponsored programs like Medicare and Medicaid. These channels are crucial for reaching diverse member segments and driving revenue. In 2023, government business alone represented about 67% of Elevance Health's total revenue, highlighting the significance of these channels.
| Channel Type | Description | Key 2024 Data/Focus |
|---|---|---|
| Direct Sales | Personalized guidance for individuals and small businesses. | Engaging members directly with plan benefits. |
| Brokers & Agents | Independent network reaching employers of all sizes. | Facilitating sales of diverse health insurance products. |
| Digital Platforms | Website and Sydney Health app for member engagement. | Investing in personalized insights and virtual care. |
| Employer Programs | Integrating plans into employee benefits packages. | Cornerstone of healthcare access for millions. |
| Government Programs | Medicare and Medicaid for specific demographics. | Medicare (65M+ beneficiaries), Medicaid (90M+ Americans) in 2024. |
| Healthcare Providers | Referrals and integrated care delivery. | 60% of revenue from health plan business in 2023, driven by network expansion. |
Customer Segments
Individuals and families represent a core customer segment for Elevance Health, seeking direct access to health insurance solutions. This includes those navigating the Affordable Care Act (ACA) marketplaces, looking for plans that align with their specific health requirements and financial capabilities. In 2024, the ACA marketplaces continued to be a significant avenue for individual coverage, with millions of Americans relying on these platforms for their health insurance needs.
Elevance Health offers tailored group health insurance and employee benefits to employer groups of all sizes, from small businesses to large corporations. This segment is crucial, encompassing both fully insured plans and self-funded options to meet diverse client needs.
In 2024, Elevance Health continued to serve a broad range of employers, with a significant portion of its revenue derived from these group health contracts. For instance, the company's employer group business is a cornerstone of its strategy, aiming to provide comprehensive and cost-effective solutions that support workforce health and productivity.
Medicare beneficiaries represent a crucial customer segment for Elevance Health, encompassing seniors and individuals eligible for Medicare due to disability or End-Stage Renal Disease. These individuals often seek robust healthcare coverage beyond traditional Original Medicare.
Elevance Health caters to this segment by offering a diverse portfolio of Medicare Advantage plans. These plans are designed to provide comprehensive medical benefits, prescription drug coverage, and often include valuable supplemental benefits like dental, vision, and hearing care, aiming to enhance overall well-being.
In 2024, Medicare Advantage enrollment continued its upward trend, with approximately 31 million beneficiaries enrolled, representing over half of the total Medicare population. This growth highlights the increasing preference for managed care options that offer predictable costs and added benefits, aligning with Elevance Health's strategy.
Medicaid Beneficiaries
Elevance Health serves Medicaid beneficiaries, a crucial customer segment encompassing low-income individuals, families, and those with disabilities across various states. This partnership with state governments highlights a commitment to accessible healthcare for vulnerable populations.
The needs of Medicaid beneficiaries are multifaceted, requiring specialized approaches to care management and health services. Elevance Health focuses on delivering tailored solutions to address these diverse requirements effectively.
- Medicaid Enrollment: In 2024, Medicaid and the Children's Health Insurance Program (CHIP) provided coverage to an estimated 94.4 million people, demonstrating the significant scale of this market.
- State Partnerships: Elevance Health operates Medicaid managed care plans in numerous states, acting as a vital partner in fulfilling state-level healthcare mandates.
- Targeted Support: The company offers specific programs and benefits designed to meet the unique health challenges faced by Medicaid enrollees, such as chronic disease management and access to preventative care.
Healthcare Providers (as partners/clients for Carelon Services)
Carelon Services partners with healthcare providers, offering them integrated care solutions, advanced data analytics, and crucial support services. This collaboration aims to streamline operations and significantly improve patient outcomes.
For instance, in 2024, Carelon's provider solutions are designed to help facilities manage complex patient populations more effectively, leading to better health results and potentially reducing readmission rates. This focus on value-based care aligns with industry trends pushing for quality over quantity.
- Integrated Care: Carelon provides tools and platforms that help providers manage patient care across different settings, from hospitals to home health.
- Data Analytics: Leveraging data, Carelon offers insights to providers to identify care gaps, optimize treatment plans, and predict patient needs.
- Support Services: This includes administrative support, technology integration, and consulting to enhance the efficiency of healthcare delivery.
- Enhanced Outcomes: The ultimate goal is to empower providers to deliver higher quality care, leading to improved patient satisfaction and clinical results.
Elevance Health's customer base is diverse, encompassing individuals and families seeking health insurance, particularly through ACA marketplaces. They also serve employer groups of all sizes, providing tailored benefits packages. A significant portion of their business involves Medicare beneficiaries, who opt for Medicare Advantage plans for enhanced coverage and supplemental benefits. Furthermore, Elevance Health is a key partner for state governments, managing Medicaid programs for low-income individuals and families.
| Customer Segment | Key Characteristics | 2024 Relevance/Data |
|---|---|---|
| Individuals & Families | Seeking direct health insurance, including ACA marketplace plans. | Millions rely on ACA marketplaces for coverage. |
| Employer Groups | Businesses of all sizes needing group health and employee benefits. | A cornerstone of revenue, providing comprehensive solutions. |
| Medicare Beneficiaries | Seniors and eligible individuals seeking robust Medicare Advantage plans. | Over half of Medicare beneficiaries (approx. 31 million in 2024) are in Medicare Advantage. |
| Medicaid Beneficiaries | Low-income individuals, families, and those with disabilities. | Estimated 94.4 million covered by Medicaid/CHIP in 2024; Elevance partners with numerous states. |
| Healthcare Providers (via Carelon) | Entities seeking integrated care, data analytics, and support services. | Focus on value-based care, improving patient outcomes and operational efficiency. |
Cost Structure
Medical benefit expenses are the most significant cost for Elevance Health, directly reflecting the price of healthcare services provided to their members. This includes everything from hospital visits and doctor appointments to the cost of prescription medications. In 2023, Elevance Health reported a Medical Loss Ratio (MLR) of 85.3%, indicating that 85.3 cents of every premium dollar went towards medical claims and quality improvements, highlighting the crucial nature of managing these costs for profitability.
Operating and administrative expenses at Elevance Health encompass a broad range of costs crucial for day-to-day operations. These include significant investments in employee compensation and benefits, the maintenance and upgrade of robust technology infrastructure, strategic marketing initiatives to reach and retain customers, and general overhead necessary to support a large organization. For instance, in 2023, Elevance Health reported selling, general, and administrative expenses of $12.4 billion, reflecting the scale of these operational outlays.
Elevance Health places a strong emphasis on disciplined expense management and the pursuit of operational efficiencies to effectively control these costs. This focus is vital for maintaining profitability and competitiveness in the healthcare industry. The company actively seeks ways to streamline processes and leverage technology to reduce administrative burdens and improve resource allocation, aiming to translate these efficiencies into better value for its members and stakeholders.
Elevance Health's CarelonRx segment incurs substantial costs related to acquiring and distributing prescription medications. These drug acquisition costs represent a major outflow, directly impacting profitability. In 2024, the pharmaceutical industry continued to see significant price fluctuations, making efficient procurement a critical challenge for CarelonRx.
Beyond the direct cost of drugs, Elevance Health also manages substantial payments to its extensive pharmacy network. These network fees are essential for ensuring broad access to medications for its members. The negotiation and management of these agreements are key to controlling overall pharmacy expenses.
Investments in Technology and Digital Solutions
Elevance Health significantly invests in technology and digital solutions as a core part of its cost structure. These investments fuel its digital transformation, encompassing areas like artificial intelligence, advanced data analytics, and robust platform development. For instance, in 2023, the company reported significant spending on technology to enhance its capabilities.
These capital expenditures are strategically deployed to achieve several key objectives. They are designed to boost operational efficiency across the organization, leading to cost savings and streamlined processes. Furthermore, these technological advancements are crucial for improving the overall member experience, making healthcare more accessible and personalized.
- Digital Transformation: Substantial investments in AI, data analytics, and platform development.
- Efficiency Gains: Aimed at streamlining operations and reducing costs.
- Member Experience: Enhancing engagement and personalization for health plan members.
- Innovation Driver: Funding R&D for new digital health solutions and services.
Acquisition and Integration Costs
Elevance Health incurs significant costs related to strategic acquisitions, a key component of its growth strategy. These expenses encompass the purchase price of target companies and the associated due diligence and legal fees. For instance, in 2023, Elevance Health completed the acquisition of CarelonRx, a pharmacy benefit manager, which involved substantial upfront investment and ongoing integration costs.
The integration of acquired businesses, such as those in home health and pharmacy services, into Elevance Health's existing operational framework represents another substantial cost driver. This includes the expenses for system migration, process harmonization, employee retraining, and ensuring compliance with Elevance Health's standards. These integration efforts are critical for realizing the full strategic and financial benefits of the acquisitions.
- Acquisition Expenses: Costs associated with identifying, valuing, and purchasing companies, including advisory and legal fees.
- Integration Costs: Expenses incurred to merge acquired businesses into Elevance Health's infrastructure, systems, and culture.
- Synergy Realization: Investments made to achieve cost savings and revenue enhancements post-acquisition, which are part of the integration process.
- Pharmacy Services Integration: Specific costs tied to integrating acquired pharmacy benefit managers and retail pharmacy operations.
Medical benefit expenses remain Elevance Health's largest cost, directly tied to the services provided to members. In 2023, the company's Medical Loss Ratio (MLR) was 85.3%, meaning the vast majority of premium revenue was spent on healthcare claims and quality initiatives, underscoring the critical need for cost management in this area.
Operating costs include significant spending on personnel, technology infrastructure, and marketing, with selling, general, and administrative expenses totaling $12.4 billion in 2023. Elevance Health actively pursues operational efficiencies to control these costs, aiming to improve resource allocation and member value.
The CarelonRx segment faces substantial drug acquisition and pharmacy network costs. In 2024, managing these expenses is particularly challenging due to ongoing price fluctuations in the pharmaceutical market, making efficient procurement a key focus.
| Cost Category | 2023 Data (USD Billions) | Notes |
| Medical Benefit Expenses | (Implied from MLR of 85.3%) | Largest cost driver, covers claims and quality improvements. |
| Selling, General & Administrative Expenses | 12.4 | Includes compensation, technology, marketing, and overhead. |
| Pharmacy Costs (CarelonRx) | Significant Outflow | Drug acquisition and pharmacy network payments. |
Revenue Streams
Elevance Health's core revenue generation hinges on health plan premiums. These premiums are collected across a diverse portfolio, encompassing employer-sponsored plans, individual market offerings, and government-backed programs like Medicare Advantage and Medicaid. The company's financial performance is directly tied to the size of its membership base and the pricing strategies for these various plans.
Elevance Health's CarelonRx segment is a significant revenue driver, primarily through its comprehensive pharmacy services. This includes the sale of prescription drugs, sophisticated formulary management to optimize drug spending, and a range of other pharmacy-related offerings.
The company reported that CarelonRx revenue increased by 9.3% in 2024, reaching $38.6 billion. This growth highlights the increasing demand for integrated pharmacy benefit management solutions and underscores its strategic importance to Elevance Health's overall financial performance.
Elevance Health's Carelon Services division is a significant revenue generator, offering a wide array of healthcare capabilities. These services cater to both Elevance's internal health plans and external customers, encompassing areas like behavioral health, comprehensive care management, and home health solutions.
In 2024, Carelon Services demonstrated robust performance, contributing substantially to Elevance Health's overall financial picture. This segment's growth is fueled by increasing demand for integrated healthcare solutions and specialized services that improve patient outcomes and operational efficiency for payers and providers alike.
Administrative Services Only (ASO) Fees
Elevance Health generates revenue through Administrative Services Only (ASO) fees, primarily from self-funded employer groups. In this model, the company acts as a service provider, managing health benefits without assuming the financial risk associated with insurance underwriting. This structure offers a predictable and consistent revenue stream.
For the fiscal year 2023, Elevance Health reported significant revenue from its ASO business. This segment is crucial for maintaining stable income, as it is less susceptible to the fluctuations often seen in traditional insurance products. The company's ability to effectively manage administrative functions for these large groups underpins this revenue generation.
- ASO Fee Revenue: Elevance Health charges administrative fees to self-funded employer groups for managing their health plans.
- Risk Mitigation: By not underwriting the insurance risk, Elevance Health secures a stable revenue base.
- 2023 Performance: The ASO segment contributed substantially to Elevance Health's overall financial performance in 2023, reflecting strong demand for these services.
Investment Income
Elevance Health earns revenue from its investment portfolio, which comprises cash reserves and various other investment assets. This investment income serves as a supplementary revenue stream, bolstering the company's overall financial performance beyond its core insurance operations.
In 2024, Elevance Health's investment income demonstrated its significance. For instance, the company reported substantial earnings from its investments, contributing positively to its bottom line.
- Investment Portfolio Income: Elevance Health capitalizes on its substantial cash and investment holdings to generate returns.
- Diversified Revenue Source: Investment income provides a crucial additional layer of revenue, enhancing financial stability.
- 2024 Performance Snapshot: The company's investment activities in 2024 yielded significant income, underscoring the importance of this revenue stream.
Beyond premiums, Elevance Health diversifies its revenue through CarelonRx, its pharmacy benefit management arm, and Carelon Services, offering a broad suite of healthcare capabilities to both internal and external clients. These segments are crucial for capturing value across the healthcare ecosystem.
The company's commitment to integrated care is evident in its revenue streams, which include administrative fees from self-funded employer groups (ASO) and income generated from its investment portfolio. This multi-faceted approach provides financial resilience.
In 2024, CarelonRx revenue grew to $38.6 billion, a 9.3% increase, showcasing strong demand for pharmacy solutions. The ASO segment also contributed significantly to overall financial performance in 2023, demonstrating stability.
| Revenue Stream | 2024 Data (if available) | 2023 Data (if available) | Notes |
|---|---|---|---|
| Health Plan Premiums | N/A | N/A | Core revenue from various health plan types. |
| CarelonRx (Pharmacy Services) | $38.6 billion (Revenue) | $35.3 billion (Approx.) | 9.3% growth in 2024. |
| Carelon Services | N/A | N/A | Broad healthcare capabilities offered internally and externally. |
| ASO Fees | N/A | Significant contribution | Fees from self-funded employer groups. |
| Investment Income | Substantial earnings | N/A | Generated from cash reserves and investment assets. |
Business Model Canvas Data Sources
The Elevance Health Business Model Canvas is informed by a comprehensive blend of financial statements, member engagement data, and regulatory filings. These sources provide a robust foundation for understanding our operations and strategic direction.
