Centene Porter's Five Forces Analysis
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
Centene Bundle
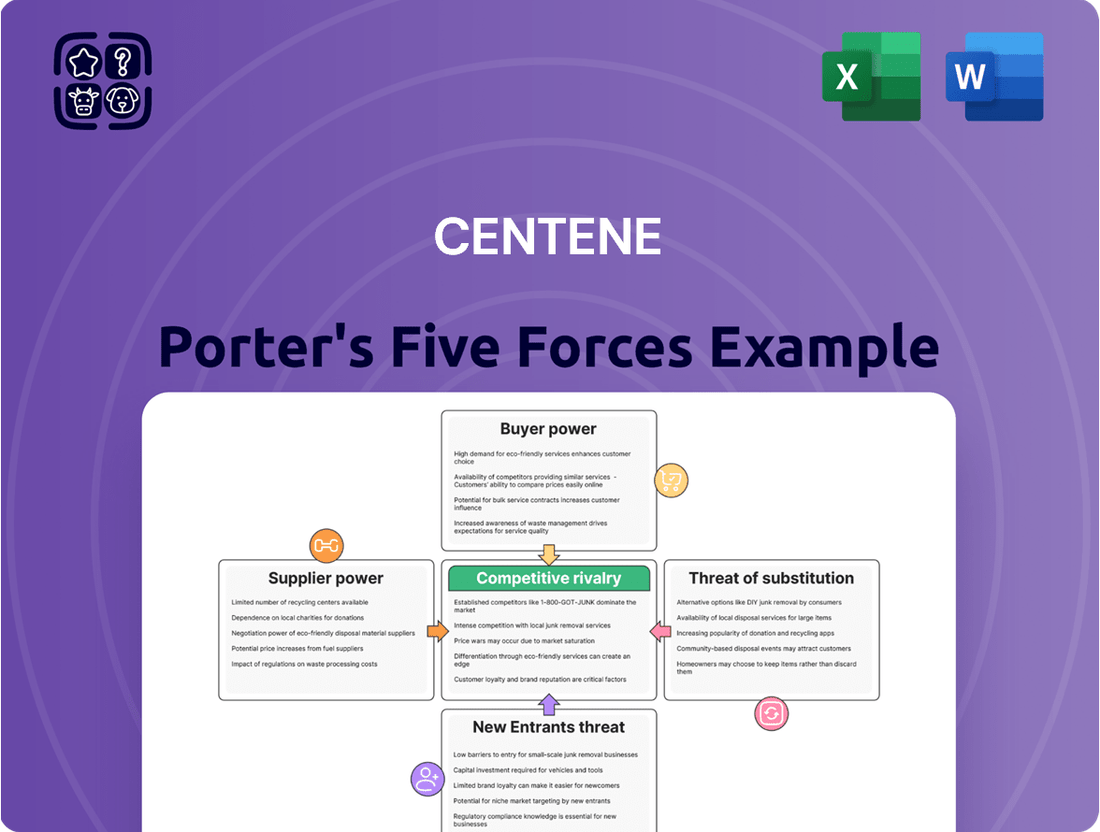
Centene operates in a complex healthcare landscape where buyer power, particularly from government programs, significantly influences pricing. The threat of new entrants is moderate, but established players leverage scale and regulatory expertise. Understanding these dynamics is crucial for navigating Centene's competitive environment.
The full analysis reveals the real forces shaping Centene’s industry—from supplier influence to threat of new entrants. Gain actionable insights to drive smarter decision-making.
Suppliers Bargaining Power
Centene's reliance on a concentrated group of specialized healthcare technology and service providers significantly boosts supplier bargaining power. The global healthcare IT market, valued at an estimated $394.8 billion in 2023, exhibits a landscape where a few dominant players cater to large organizations like Centene, granting these suppliers considerable leverage.
Centene's reliance on a limited number of pharmaceutical companies and medical equipment manufacturers significantly amplifies supplier bargaining power. For instance, in 2024, the top three pharmaceutical suppliers to the healthcare industry collectively held over 60% of the market share for critical medications, giving them considerable leverage over pricing and terms.
This dependency means that these suppliers can dictate terms, potentially leading to higher costs for Centene. When a company like Centene needs specific, often patented, drugs or specialized medical devices, it has fewer alternatives, making it harder to negotiate favorable pricing or supply agreements.
Centene faces significant complexity when negotiating contracts with healthcare network providers. These negotiations are lengthy, often spanning 4-6 months, and require substantial time and resources. The frequency of renegotiations, typically every 2-3 years, adds to this ongoing challenge.
The intricate nature of these contract discussions, combined with Centene's critical need to maintain a broad and robust provider network, can significantly amplify the bargaining power of healthcare providers. This leverage allows them to potentially dictate more favorable terms, impacting Centene's operational costs and network accessibility.
Significant Investment Required to Switch Suppliers
Centene faces a significant hurdle in switching its core technology platforms or other critical suppliers. The estimated costs for migrating these platforms can range from $15 million to $25 million, with implementation timelines stretching between 12 to 18 months. This substantial financial and operational commitment makes it challenging for Centene to readily change its supplier relationships.
The potential for revenue disruption during such a transition further amplifies the bargaining power of existing suppliers. Centene could experience revenue impacts estimated between $50 million and $75 million if a supplier switch is not managed flawlessly. This risk inherently strengthens the position of incumbent suppliers, as the cost and complexity of switching are considerable deterrents.
- High Switching Costs: Migrating core technology platforms for Centene involves substantial financial outlays, estimated at $15-25 million.
- Extended Implementation Periods: The process of switching suppliers can take a considerable 12-18 months, disrupting ongoing operations.
- Revenue Disruption Risk: Potential revenue losses of $50-75 million during transitions empower suppliers by highlighting the consequences of change.
Regulatory Requirements and Compliance Costs
Suppliers of services and products to Centene must navigate a complex web of healthcare regulations, including ongoing updates to HIPAA and other evolving compliance mandates. Meeting these stringent demands requires significant investment in technology, personnel, and ongoing training, which can be a barrier for smaller or less sophisticated suppliers.
This regulatory burden effectively limits the pool of qualified suppliers capable of serving Centene. Consequently, those suppliers who can meet and maintain these high compliance standards often command higher prices for their goods and services, thereby increasing their bargaining power.
For instance, the cost of ensuring data privacy and security under HIPAA can be substantial. In 2024, healthcare organizations are expected to continue investing heavily in cybersecurity measures, with the global healthcare cybersecurity market projected to reach significant figures, indicating the high cost of compliance that suppliers must absorb and pass on.
- Increased Compliance Burden: Suppliers face escalating costs and operational complexities to adhere to evolving healthcare regulations.
- Limited Supplier Pool: Stringent requirements naturally reduce the number of qualified and compliant vendors available to Centene.
- Cost Pass-Through: Suppliers pass on their compliance-related expenses, enhancing their pricing power and thus their bargaining leverage.
Centene's bargaining power with suppliers is notably constrained by high switching costs for critical services, such as technology platforms, which can range from $15 million to $25 million and take 12-18 months to implement. This inertia, coupled with the risk of significant revenue disruption, estimated between $50 million and $75 million during transitions, grants incumbent suppliers considerable leverage over pricing and terms.
The stringent regulatory environment in healthcare, including HIPAA compliance, further limits Centene's supplier options. Suppliers must invest heavily in technology and personnel to meet these demands, a cost that is often passed on through higher prices. This creates a scenario where a smaller pool of qualified vendors can dictate terms, impacting Centene's procurement costs.
| Factor | Centene Impact | Supplier Leverage |
|---|---|---|
| Switching Costs (Technology) | $15M - $25M | High |
| Implementation Time | 12 - 18 months | High |
| Potential Revenue Disruption | $50M - $75M | High |
| Regulatory Compliance Burden | Increased Supplier Costs | Moderate to High |
| Concentration of Specialized Suppliers | Limited Alternatives | High |
What is included in the product
This analysis unpacks the competitive forces impacting Centene, including the bargaining power of buyers and suppliers, the threat of new entrants and substitutes, and the intensity of rivalry within the managed care industry.
Easily identify and mitigate competitive threats with a structured framework that simplifies complex market dynamics.
Gain actionable insights into industry profitability by pinpointing key areas of leverage and vulnerability.
Customers Bargaining Power
Centene's primary customer base consists of government-sponsored healthcare programs, specifically Medicaid and Medicare. This means federal and state governments wield substantial bargaining power. Their immense purchasing volume, as demonstrated by Medicare's estimated $884 billion in spending for 2023, allows them to dictate terms and reimbursement rates, significantly impacting Centene's revenue and profitability.
Government-sponsored healthcare markets, such as Medicaid and Medicare, exhibit significant price sensitivity. Regulators impose strict medical loss ratios (MLRs), typically between 85% and 88%, which directly limit how much Centene can spend on administrative costs and profit, forcing a focus on cost containment.
This stringent regulatory environment means Centene faces continuous pressure on its pricing strategies and profit margins. The mandated MLRs effectively cap profitability, making efficient operations and cost management paramount for success in these crucial markets.
Changes in federal legislation, like proposed Medicaid funding cuts or alterations to Affordable Care Act subsidies, directly influence Centene's customer base and their purchasing power for health coverage. For example, the 2025 Budget Reconciliation Act is projected to leave as many as 15 million more individuals uninsured by 2034, a shift that could dramatically reshape the customer market.
Customer Choice and Accessibility in Health Insurance Marketplaces
Centene operates within the Health Insurance Marketplace, a segment where customer choice is a significant factor. As of 2024, the number of qualified health plans available on the HealthCare.gov platform, which serves many states, continues to offer consumers a range of options. This variety directly impacts customer bargaining power, as individuals can compare benefits, premiums, and provider networks.
The ability for customers to switch plans annually during open enrollment periods, or even mid-year due to qualifying life events such as marriage or job loss, further amplifies their leverage. For instance, in 2024, the Centers for Medicare & Medicaid Services (CMS) reported millions of individuals enrolled in marketplace plans, many of whom had multiple plan choices during the enrollment period.
- Increasing Plan Availability: The Health Insurance Marketplace offers a growing number of plan options, allowing consumers to select coverage that best fits their needs and budget.
- Switching Flexibility: Customers can change their health insurance plans during open enrollment or following specific life events, enhancing their ability to seek better value.
- Impact of Subsidies: Changes in government subsidies can influence customer decisions and their price sensitivity, indirectly affecting their bargaining power.
- Consumer Information: Greater access to information about plan performance and costs empowers consumers to make more informed choices and negotiate better terms.
Influence of Member Acuity and Risk Adjustment on Pricing
The bargaining power of customers in the ACA marketplace is significantly shaped by their health status, or acuity, and the subsequent risk adjustment payments insurers receive. Centene, for instance, faces increased costs when serving members with higher health needs, as these individuals typically require more medical services. This dynamic directly influences how much insurers can effectively charge or how much they are compensated for providing coverage.
In 2024, Centene experienced this pressure firsthand. The company reported that shifts in member demographics, with a greater influx of sicker individuals and an outflow of healthier ones, contributed to substantial financial strain. This meant that the average cost of care per member increased, effectively raising the 'price' Centene had to absorb for serving its customer base.
- Member Acuity Impact: Higher health needs among ACA marketplace members directly translate to increased healthcare utilization and, consequently, higher costs for insurers like Centene.
- Risk Adjustment Mechanism: The health status of members influences risk adjustment payments, which are designed to compensate insurers for covering higher-cost individuals.
- Centene's 2024 Experience: In 2024, Centene faced financial pressure due to a trend of enrolling members with greater health needs and losing healthier individuals, escalating the cost of serving its customer base.
Centene's customer base, primarily government programs like Medicaid and Medicare, grants these entities immense bargaining power. Their sheer purchasing volume, exemplified by Medicare's projected $900 billion in spending for 2024, allows them to dictate terms and reimbursement rates, directly impacting Centene's revenue.
The competitive landscape of the Health Insurance Marketplace also empowers customers. With numerous plan options available on platforms like HealthCare.gov in 2024, consumers can readily compare benefits and costs, driving price sensitivity and the ability to switch plans annually. This flexibility enhances their leverage.
Centene's 2024 experience highlighted the impact of member acuity. A shift towards enrolling individuals with greater health needs, while losing healthier members, increased the average cost of care per member, demonstrating how customer health status directly affects insurer profitability and pricing power.
| Customer Segment | Bargaining Power Factor | Impact on Centene | Supporting Data (2024/2025 Estimates) |
|---|---|---|---|
| Government Programs (Medicaid/Medicare) | High Purchasing Volume, Price Regulation | Dictates reimbursement rates, limits profit margins | Medicare spending estimated at $900 billion (2024) |
| Health Insurance Marketplace Consumers | Plan Availability, Switching Flexibility | Drives price competition, necessitates value proposition | Millions enrolled on HealthCare.gov, multiple plan choices |
| Member Health Status (Acuity) | Risk Adjustment Payments, Cost of Care | Increases per-member costs, strains profitability | Centene reported increased costs due to sicker member influx in 2024 |
Preview the Actual Deliverable
Centene Porter's Five Forces Analysis
This preview showcases the complete Centene Porter's Five Forces Analysis, detailing the competitive landscape of the managed care industry. You're looking at the actual document; once you complete your purchase, you’ll get instant access to this exact, professionally written analysis, providing a thorough understanding of industry rivalry, the bargaining power of buyers and suppliers, the threat of new entrants, and the threat of substitute products.
Rivalry Among Competitors
Centene faces intense competition from major national healthcare companies like UnitedHealth Group, Elevance Health, Humana, and Cigna Group. These giants possess significant resources and established market presence, directly challenging Centene's ability to gain and retain members across diverse health insurance offerings.
In 2024, the healthcare insurance market remains a battleground, with these large competitors frequently engaging in aggressive pricing strategies and innovative product development to capture market share. For instance, UnitedHealth Group reported revenues exceeding $370 billion in 2023, demonstrating the sheer scale and competitive power Centene must contend with.
Centene's core business revolves around government-sponsored programs like Medicaid, Medicare, and Health Insurance Marketplace plans. This focus inherently places it in direct competition with other insurers that also specialize in these regulated markets. For instance, in 2023, the Medicaid redetermination process, which reassures eligibility for millions, created significant churn and intensified competition as insurers vied to retain or acquire members.
The competitive landscape is further sharpened by state-level contract reprocurements, where Centene, like its rivals, must continually bid for the right to serve members within specific states. This process often involves intense price competition and service level negotiations. The ongoing impact of Medicaid redeterminations, which began in 2023 and continued through 2024, has also been a major factor, leading to shifts in membership and increased efforts by competitors to capture market share.
Competitors in the health insurance sector, particularly within the Affordable Care Act (ACA) marketplace, frequently employ aggressive pricing tactics to win over new members. This can manifest as offering very low-cost or even $0 premium plans, which, while effective for boosting enrollment numbers, can significantly squeeze profit margins for all players in the market.
Centene, for instance, has historically leveraged these low-price strategies to expand its membership base. In 2023, Centene reported a medical loss ratio of 89.4%, indicating that a substantial portion of its revenue was spent on healthcare claims, a figure that can be further strained by intense price competition.
Impact of Regulatory and Policy Changes on Competition
The healthcare insurance sector, particularly for companies like Centene that focus on government-sponsored programs, is heavily influenced by regulatory shifts. Changes in Medicaid funding, Affordable Care Act (ACA) subsidies, and Medicare Advantage reforms directly impact profitability and market access. For instance, in 2024, ongoing discussions around Medicaid managed care rate setting and potential adjustments to federal matching rates create uncertainty, forcing insurers to meticulously manage their bids and operational costs.
These policy changes can rapidly alter the competitive dynamics. For example, an increase in ACA subsidies might broaden the market for individual plans, creating opportunities for insurers with robust networks and competitive pricing. Conversely, stricter regulations on provider reimbursement or benefit mandates can squeeze margins, potentially leading to market exits or consolidation. Centene, as a major player in Medicaid and Medicare, must constantly recalibrate its strategy to adapt to these evolving policy landscapes, which are crucial for its competitive positioning.
- Medicaid Funding: Federal Medical Assistance Percentage (FMAP) rates, which determine the federal share of Medicaid costs, are subject to periodic review and potential adjustments, directly impacting state budgets and managed care capitation rates.
- ACA Subsidies: The continuation and level of premium tax credits under the ACA significantly influence enrollment numbers and affordability for the individual market, a segment where Centene has expanded its presence.
- Medicare Reforms: Changes to the Medicare Advantage Star Ratings program and payment methodologies can affect the competitive attractiveness and profitability of Medicare plans offered by insurers.
- State-Specific Regulations: Beyond federal policies, individual states often implement their own regulatory frameworks for health insurers, affecting everything from network adequacy to marketing practices, adding another layer of complexity to competition.
Innovation and Technology Investment as a Competitive Differentiator
Centene, like many healthcare giants, is pouring significant resources into technology and innovation, particularly artificial intelligence (AI). This investment aims to streamline operations, cut costs, and elevate the member experience. For instance, in 2024, Centene continued its focus on digital transformation, leveraging AI for tasks like claims processing and member outreach, which directly impacts their ability to compete on efficiency and service quality.
This technological edge is becoming a crucial differentiator in the highly competitive health insurance landscape. Companies with substantial scale, such as Centene, can make larger, more impactful investments in these areas. This allows them to develop sophisticated data analytics capabilities that can predict health trends, personalize member care plans, and optimize network performance, setting them apart from smaller or less technologically advanced rivals.
- Centene's 2024 technology investments are geared towards AI for operational efficiency and enhanced member services.
- Scale advantage allows large players like Centene to out-invest competitors in technological advancements.
- Data analytics derived from these investments provide a competitive edge in personalized care and predictive health insights.
Centene operates in a fiercely competitive market, facing off against industry titans like UnitedHealth Group and Elevance Health, which boast substantial financial resources and established market positions. This intense rivalry is particularly evident in 2024 as major players engage in aggressive pricing and product innovation to capture market share, with UnitedHealth Group's 2023 revenue exceeding $370 billion underscoring the scale of competition.
The company's focus on government-sponsored programs such as Medicaid and Medicare places it in direct competition with other specialized insurers, especially during periods of significant membership change like the Medicaid redeterminations that continued through 2024. This process has intensified the battle for members, with insurers actively seeking to retain or acquire new enrollees.
| Competitor | 2023 Revenue (approx.) | Key Business Areas |
|---|---|---|
| UnitedHealth Group | $371.3 billion | Managed care, health services |
| Elevance Health | $171.8 billion | Managed care, pharmacy benefit management |
| Humana | $103.1 billion | Managed care, military care |
| Cigna Group | $187.5 billion | Managed care, pharmacy services |
SSubstitutes Threaten
A significant substitute for Centene's managed care services is direct government healthcare provision. This involves states or the federal government managing health programs internally rather than outsourcing to private companies like Centene. While private managed care organizations are prevalent, this direct model remains a potential alternative that could reduce reliance on third-party providers.
For instance, in 2024, many states continue to operate or explore options for directly managing Medicaid populations, especially for specific services or populations. This can be seen as a competitive threat if governments find it more cost-effective or efficient to handle these functions in-house, bypassing the administrative fees and profit margins associated with managed care organizations. The trend towards greater state control over healthcare delivery could intensify this substitute threat.
Self-funded employer plans present a significant threat to Centene, as they allow companies to directly manage and bear the risk of their employees' healthcare costs, bypassing traditional insurance carriers. This can be particularly appealing for larger employers seeking greater control and potential cost savings.
Alternative coverage models, such as Individual Coverage Health Reimbursement Arrangements (ICHRAs), also act as substitutes. ICHRAs empower employees to purchase their own health insurance, with employers contributing a set amount, offering flexibility and potentially lower administrative burdens for businesses.
Centene itself views ICHRA as a market disruption, acknowledging its potential to draw individuals away from fully insured plans. This strategic recognition underscores the competitive pressure these alternative models exert on Centene's core business.
The growing popularity of direct primary care (DPC) and cash-pay models presents a significant threat of substitution for Centene. These alternatives allow patients, particularly those with disposable income or who are uninsured, to bypass traditional insurance networks for routine and preventative care. For example, DPC practices often charge a flat monthly fee, offering more predictable costs and direct access to physicians, which can be appealing compared to the complexities and co-pays associated with managed care plans.
Non-Traditional Health and Wellness Programs
The increasing focus on preventative care and wellness initiatives, often provided by employers or community groups, presents a significant threat of substitutes for traditional health insurance providers like Centene. These programs aim to keep individuals healthy, thereby potentially reducing their reliance on extensive insurance coverage. For instance, a growing number of companies are investing in on-site fitness centers or offering subsidies for gym memberships, as seen in the 2024 trend where corporate wellness spending saw a notable uptick.
These non-traditional programs directly address health maintenance, offering alternatives that bypass the need for extensive medical interventions often covered by insurance. This can lead to a decrease in demand for certain insurance products. Data from 2024 indicates a rising participation rate in employer-sponsored wellness challenges, with some studies showing a correlation between participation and reduced healthcare claims.
- Employer-sponsored wellness programs are gaining traction, with many companies increasing their investment in preventative health measures for employees.
- Community-based health initiatives and digital wellness platforms offer accessible and often lower-cost alternatives for managing personal health.
- The emphasis on lifestyle changes and early intervention through these programs can diminish the perceived necessity of comprehensive health insurance for some individuals.
Shifts in Public Health Initiatives and Community Support
Enhanced public health initiatives and community support systems, especially for vulnerable groups, can lessen the need for extensive health insurance by tackling social determinants of health and offering fundamental care. For instance, in 2024, many cities are expanding community health worker programs, aiming to improve preventative care access. These programs often focus on areas like nutrition and housing assistance, directly impacting health outcomes.
Centene actively participates in collaborations with non-profit organizations to bolster access to healthy food and economic stability. These partnerships, which saw significant growth in 2023 and continued into 2024, aim to address root causes of poor health. By improving these social determinants, Centene indirectly reduces the demand for certain healthcare services that might otherwise be necessary.
- Community Health Worker Expansion: Many urban areas are increasing funding for community health worker programs in 2024, with a focus on preventative care and chronic disease management.
- Partnerships for Social Determinants: Centene reported in its 2023 annual filings that it expanded its network of community-based partnerships by 15%, specifically targeting food security and housing initiatives.
- Impact on Healthcare Utilization: Early data from pilot programs in 2023 suggests a potential 5-10% reduction in emergency room visits for participants in integrated social support programs.
The threat of substitutes for Centene's offerings is multifaceted, encompassing direct government provision, self-funded employer plans, and direct primary care models. These alternatives can bypass traditional managed care, offering potential cost savings and greater control. For example, in 2024, many states are exploring direct management of Medicaid populations, and companies are increasingly adopting self-funded plans. Furthermore, the rise of cash-pay models and wellness programs directly addresses health maintenance, potentially reducing the perceived need for comprehensive insurance.
| Substitute Type | Description | 2024 Trend/Data Point |
|---|---|---|
| Direct Government Provision | States or federal government managing healthcare directly. | Continued exploration by states to manage Medicaid populations internally. |
| Self-Funded Employer Plans | Companies directly manage and bear employee healthcare costs. | Increasing adoption by larger employers seeking cost control and flexibility. |
| Direct Primary Care (DPC) | Flat monthly fees for direct patient-physician access. | Growing popularity for routine and preventative care, offering predictable costs. |
| Wellness Programs | Employer-sponsored or community initiatives focusing on preventative health. | Notable uptick in corporate wellness spending in 2024; increased participation in wellness challenges. |
Entrants Threaten
The healthcare insurance sector is characterized by formidable regulatory hurdles, acting as a significant deterrent to new entrants. Companies must navigate a complex web of state and federal laws, including rigorous licensing and accreditation processes. For instance, the Centers for Medicare & Medicaid Services (CMS) imposes strict operational and financial requirements for participation in government programs, demanding substantial upfront investment and ongoing compliance efforts.
Establishing a health insurance company, particularly one focused on government programs like Centene, requires immense upfront capital. Think millions, if not billions, for robust IT infrastructure, building out extensive provider networks, and setting up the necessary administrative backbone. For instance, in 2024, the average cost to launch a health insurance startup in the US can easily exceed $50 million, a significant hurdle for any newcomer.
New entrants face a significant hurdle in building extensive provider networks, a critical component for attracting and serving members in the health insurance market. This process is time-consuming and complex, requiring substantial investment and relationship-building over many years.
Established players like Centene have already forged deep, long-standing relationships with a vast array of healthcare providers. Replicating this comprehensive network, which includes hospitals, physicians, and specialists across diverse geographic areas, presents a formidable barrier for any newcomer aiming to compete effectively.
Brand Recognition and Customer Trust
Existing players like Centene benefit from established brand recognition and customer trust, particularly among vulnerable populations served by Medicaid and Medicare. New entrants would need considerable time and investment to build comparable levels of trust and market presence.
For instance, in 2023, Centene's brand awareness among its core demographic was a significant asset, with surveys indicating a preference for familiar providers. Replicating this trust requires substantial marketing efforts and a proven track record of reliable service delivery.
- Brand Loyalty: Centene's long-standing presence fosters loyalty, making it harder for newcomers to attract members.
- Reputational Capital: Trust built over years in serving government-sponsored health plans is a formidable barrier.
- Customer Acquisition Cost: New entrants face high costs to acquire customers who are accustomed to Centene's services.
- Market Penetration: Achieving the widespread market penetration Centene enjoys would demand extensive outreach and infrastructure development.
Policy and Funding Volatility in Government Programs
The threat of new entrants into the managed care sector, particularly for companies reliant on government programs, is significantly mitigated by the inherent volatility and uncertainty in policy and funding. Recent shifts in Medicaid and the Affordable Care Act (ACA) demonstrate how quickly the landscape can change, making it a less predictable environment for newcomers.
This policy and funding volatility acts as a substantial barrier. For instance, changes in reimbursement rates or eligibility criteria, which have been frequent in recent years, can drastically alter a company's revenue streams and profitability. This risk of sudden, impactful policy shifts deters potential new entrants who might otherwise be attracted to the scale of government healthcare programs.
- Policy Uncertainty: Fluctuations in government healthcare policies, such as recent adjustments to Medicaid expansion or ACA subsidies, create an unpredictable operating environment.
- Funding Volatility: Shifts in government funding levels for healthcare programs can directly impact the financial viability of new entrants.
- Deterrent to Entry: The risk of adverse policy changes and funding cuts discourages new companies from investing heavily in a market with such inherent instability.
The threat of new entrants in Centene's market is low due to substantial capital requirements, extensive provider network development, and established brand loyalty. Regulatory complexities, such as stringent licensing and compliance with CMS requirements, also pose significant barriers. The inherent policy and funding volatility within government-sponsored health programs further deters new companies from entering this space. For example, in 2024, the estimated startup cost for a US health insurance company can exceed $50 million, a figure that underscores the immense capital needed.
| Barrier | Description | Impact on New Entrants | Centene Advantage |
|---|---|---|---|
| Capital Requirements | High upfront investment for infrastructure and operations. | Significant hurdle for startups. | Established financial resources. |
| Provider Networks | Time-consuming and costly to build comprehensive networks. | Difficult to match existing breadth and depth. | Extensive, long-standing provider relationships. |
| Brand Recognition & Trust | Building customer loyalty and reputation takes years. | Challenging to attract members from established players. | Strong brand awareness and trust, especially with vulnerable populations. |
| Regulatory Compliance | Navigating complex state and federal healthcare laws. | Requires significant legal and operational expertise. | Experienced in managing complex regulatory landscapes. |
| Policy/Funding Volatility | Uncertainty in government program rules and funding. | Increases risk for new investors. | Adaptability and experience managing policy shifts. |
Porter's Five Forces Analysis Data Sources
Our Centene Porter's Five Forces analysis is built upon a foundation of comprehensive data, including Centene's annual reports and SEC filings, alongside industry-specific market research from sources like IBISWorld and Statista. We also incorporate insights from government health databases and competitor financial disclosures to provide a robust competitive landscape.
