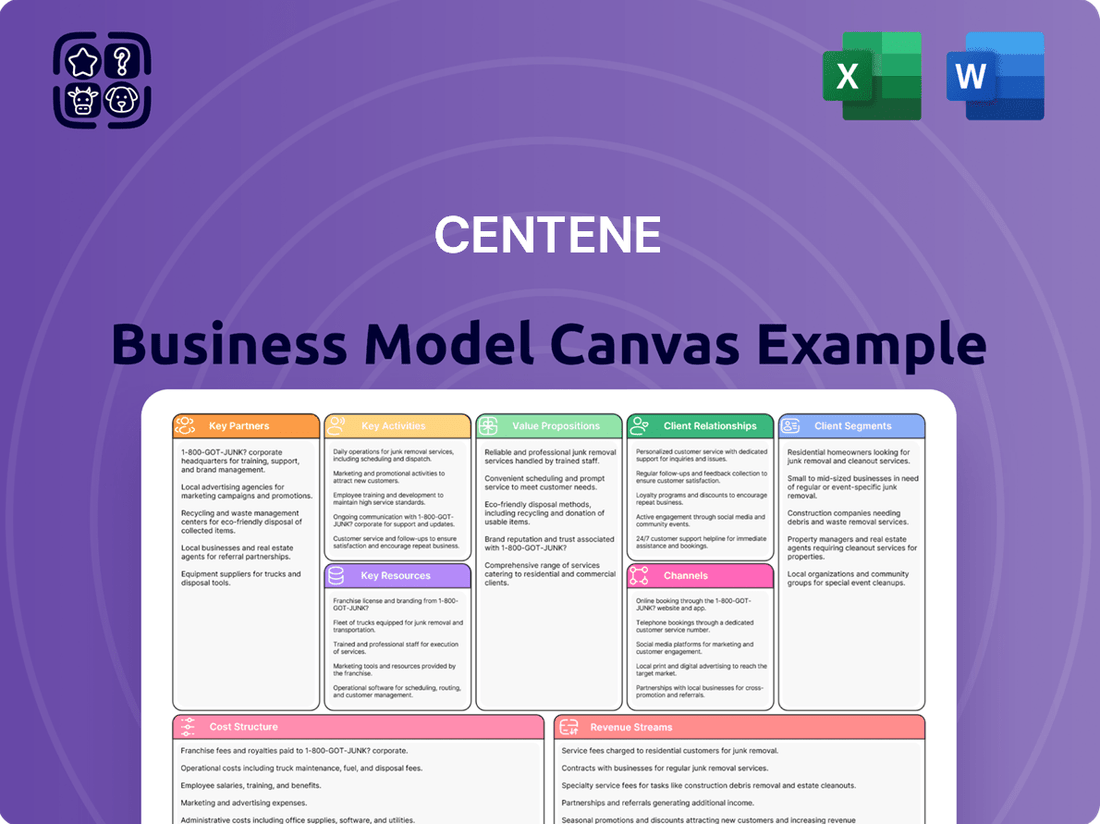
Centene Business Model Canvas
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
Centene Bundle
Discover the strategic framework behind Centene's success with our comprehensive Business Model Canvas. This detailed breakdown illuminates their key customer segments, value propositions, and revenue streams, offering a clear picture of how they navigate the healthcare landscape.
Unlock the full strategic blueprint behind Centene's business model. This in-depth Business Model Canvas reveals how the company drives value, captures market share, and stays ahead in a competitive landscape. Ideal for entrepreneurs, consultants, and investors looking for actionable insights.
Partnerships
Centene's core operations are deeply intertwined with government agencies like the Centers for Medicare & Medicaid Services (CMS). These partnerships are essential for Centene to administer vital programs such as Medicaid, Medicare, and plans offered through the Health Insurance Marketplace. For instance, in 2024, Centene continued to be a major player in state Medicaid programs, managing care for millions of beneficiaries.
Centene builds extensive networks of healthcare providers, including hospitals, physicians, and clinics, to serve its members. These collaborations are vital for guaranteeing access to quality care and managing costs.
In 2024, Centene continued to focus on strengthening these provider relationships. For instance, the company actively works to integrate new providers into its network to meet the evolving needs of its government-sponsored health plan members.
Centene's strategic alliances with Pharmacy Benefit Managers (PBMs) and a broad network of retail pharmacies are fundamental to its operational success. These partnerships are critical for efficiently administering prescription drug benefits, ensuring that Centene's members can access their prescribed medications reliably.
The company's in-house specialty pharmacies, including AcariaHealth and PANTHERx, are integral to this strategy. These operations not only provide specialized medication services but also actively manage drug costs and improve patient outcomes, contributing significantly to Centene's value proposition.
Community Organizations and Social Service Agencies
Centene actively partners with community organizations and social service agencies to tackle social determinants of health, or SDOH. These collaborations are crucial for connecting members with essential non-medical resources. For instance, in 2024, Centene's initiatives focused on expanding access to food security programs, with a goal of serving an additional 50,000 individuals through these partnerships by year-end.
These partnerships are designed to provide holistic support, going beyond traditional healthcare to address needs like housing stability and reliable transportation. Such interventions are recognized as vital for improving overall health outcomes. In 2023, Centene reported that members engaged with these community resources showed a 15% higher adherence rate to preventative care screenings.
- Addressing Food Insecurity: Partnerships with food banks and community kitchens aim to reduce hunger among vulnerable populations.
- Housing Support: Collaborations with housing assistance programs help members secure stable and safe living environments.
- Transportation Solutions: Working with local transit authorities and ride-sharing services ensures members can access healthcare appointments and essential services.
Technology and Digital Health Solution Providers
Centene actively collaborates with technology and digital health solution providers to navigate the evolving healthcare landscape. These partnerships are crucial for developing and implementing innovative solutions that improve member care and operational effectiveness. For instance, in 2024, Centene continued to invest in digital platforms aimed at enhancing member engagement and providing more accessible care options.
These collaborations span a range of critical areas. They include the development of advanced telemedicine platforms, sophisticated data analytics tools for better population health management, and integrated systems for seamless care coordination. Such partnerships allow Centene to leverage cutting-edge technology to streamline its operations and deliver more personalized and efficient healthcare services to its diverse membership.
Key areas of partnership include:
- Telemedicine Platforms: Enhancing virtual access to healthcare providers.
- Data Analytics Solutions: Utilizing big data for predictive health insights and personalized interventions.
- Care Coordination Tools: Integrating patient data across different care settings for smoother transitions.
- Digital Engagement Apps: Empowering members with tools for health management and communication.
Centene’s key partnerships are foundational to its business model, enabling it to effectively serve government-sponsored health plan members. These relationships span critical areas from government agencies and healthcare providers to pharmaceutical benefit managers and community organizations.
In 2024, Centene continued to deepen its engagement with state Medicaid agencies, managing care for millions of beneficiaries. The company also focused on expanding its network of healthcare providers, ensuring access to quality care and cost management for its members.
Strategic alliances with Pharmacy Benefit Managers (PBMs) and a vast network of retail pharmacies are vital for efficient prescription drug benefit administration. Furthermore, collaborations with community organizations address social determinants of health, enhancing member well-being through support for food security, housing, and transportation.
Centene also partners with technology providers to implement innovative solutions like telemedicine and advanced data analytics, aiming to improve member engagement and operational efficiency in 2024.
| Partner Type | 2024 Focus/Activity | Impact |
|---|---|---|
| Government Agencies (CMS, State Medicaid) | Administering Medicaid, Medicare, Marketplace plans | Core revenue generation, program compliance |
| Healthcare Providers (Hospitals, Physicians) | Network expansion, integrated care models | Ensured access to care, cost containment |
| Pharmacy Benefit Managers (PBMs) & Pharmacies | Prescription drug benefit management | Efficient medication access, cost optimization |
| Community Organizations & Social Services | Addressing Social Determinants of Health (SDOH) | Improved member outcomes, holistic support |
| Technology & Digital Health Providers | Telemedicine, data analytics development | Enhanced member engagement, operational efficiency |
What is included in the product
This Centene Business Model Canvas provides a detailed overview of their strategy, focusing on government-sponsored healthcare programs and their diverse customer segments, value propositions, and key partnerships.
It offers a comprehensive analysis of Centene's operations, channels, and revenue streams, designed to inform strategic decisions and stakeholder discussions.
Centene's Business Model Canvas acts as a pain point reliever by providing a clear, visual representation of how they deliver affordable healthcare, addressing the complexity of managing diverse member needs and regulatory landscapes.
Activities
Centene's core activities revolve around the meticulous management and administration of diverse health plans. This encompasses everything from enrolling new members and processing claims efficiently to providing robust member services and ensuring strict adherence to regulatory compliance across Medicaid, Medicare, and Health Insurance Marketplace programs.
In 2024, Centene's commitment to operational excellence in plan management is critical. For instance, the company serves millions of members, and the seamless processing of billions of dollars in claims annually underpins its ability to deliver value and maintain member satisfaction while navigating complex government program rules.
Centene actively cultivates and oversees its vast network of healthcare providers, a crucial element for delivering comprehensive care. This involves establishing contracts with hospitals, physicians, and various healthcare facilities, alongside rigorous credentialing processes to ensure quality and access.
A key focus is on building and maintaining relationships with providers, ensuring they meet Centene's standards for patient care and service delivery. This proactive management is vital for member satisfaction and operational efficiency.
In 2024, Centene continued to emphasize value-based care arrangements, aiming to improve health outcomes and manage costs effectively. This strategy involves aligning provider incentives with quality metrics and patient well-being, fostering a more coordinated approach to healthcare delivery.
Centene's key activities revolve around actively managing member health through targeted programs. This includes implementing care coordination strategies and preventative health initiatives designed to improve overall health outcomes, particularly for vulnerable populations. In 2024, Centene continued to focus on these areas, aiming to reduce hospital readmissions and manage chronic diseases more effectively across its diverse membership base.
Cost Management and Risk Adjustment
Centene's cost management hinges on aggressive provider rate negotiations and robust utilization management programs. These efforts aim to control the escalating costs inherent in healthcare delivery. For instance, in 2024, Centene continued to refine its value-based care arrangements, seeking to align provider incentives with quality outcomes and cost efficiency.
Risk adjustment is a cornerstone of Centene's operations, especially within its Marketplace business. This process involves sophisticated data analytics to accurately capture the health conditions of its member base. This ensures that the company receives appropriate capitation payments that reflect the actual healthcare needs of its enrollees, a critical factor for financial sustainability.
- Provider Rate Negotiation: Centene actively negotiates reimbursement rates with its network of healthcare providers to manage overall medical expenses.
- Utilization Management: Implementing programs that review and manage the necessity and appropriateness of healthcare services to control costs.
- Risk Adjustment Accuracy: Ensuring precise coding and data submission to accurately reflect member health status and secure adequate funding, particularly vital in government-sponsored programs.
- Value-Based Care Initiatives: Shifting towards payment models that reward providers for quality and cost-effectiveness, aligning with industry trends.
Regulatory Compliance and Government Relations
Centene’s operations are deeply intertwined with government-sponsored healthcare programs, making regulatory compliance a paramount activity. This involves constant monitoring and adherence to evolving federal and state healthcare laws and regulations. For instance, in 2024, the company continued to navigate complex requirements for Medicare Advantage and Medicaid managed care plans, which are subject to significant oversight from agencies like the Centers for Medicare & Medicaid Services (CMS).
Maintaining robust government relations is crucial for Centene’s success. This includes actively engaging with policymakers and regulatory bodies to understand and influence healthcare policy. It also ensures Centene's participation and success in competitive procurement processes for state contracts, which are vital for securing and expanding its member base in government programs. In 2024, Centene actively participated in numerous state contract bids, a common practice for health insurers in this sector.
- Regulatory Adherence: Ensuring all operations, from plan design to claims processing, meet the stringent standards set by federal and state health agencies.
- Policy Engagement: Participating in public comment periods and legislative discussions to advocate for policies that support accessible and affordable healthcare.
- Contract Procurement: Successfully bidding for and securing contracts with state governments to administer Medicaid and other managed care programs.
- Compliance Monitoring: Implementing systems and processes to continuously track and report on compliance with program rules and quality metrics.
Centene's key activities are centered on managing health insurance plans, particularly for government-sponsored programs. This involves member enrollment, claims processing, and providing customer support, all while adhering to strict regulations. In 2024, the company managed millions of members, processing billions in claims, underscoring the scale of its administrative operations.
Preview Before You Purchase
Business Model Canvas
The Centene Business Model Canvas preview you see is the actual document you will receive upon purchase. This means the structure, content, and formatting are identical to the final deliverable, ensuring no surprises. You can be confident that what you preview is precisely what you will get, ready for your immediate use.
Resources
Centene's extensive provider networks are a cornerstone of its business, encompassing a wide array of hospitals, clinics, and individual practitioners. This vast network is crucial for delivering comprehensive healthcare services to its members. For instance, as of the first quarter of 2024, Centene served approximately 6.8 million Medicaid members, requiring a robust network to meet their diverse healthcare needs across numerous states.
The sheer scale of these provider relationships allows Centene to offer a broad spectrum of medical, behavioral, and specialized care. This deep penetration into local healthcare markets is a significant competitive advantage, ensuring members have access to necessary treatments and services. By contracting with over 600,000 providers nationally by the end of 2023, Centene demonstrates its commitment to accessibility and quality care delivery.
Centene's human capital is a cornerstone, featuring a vast and skilled workforce. This includes a significant number of medical professionals, dedicated care managers, essential administrative staff, and crucial IT specialists. Their collective expertise is fundamental to navigating the intricacies of health plan management and ensuring seamless member support.
In 2023, Centene employed approximately 72,000 associates. This substantial team is the engine behind their operational efficiency and their ability to manage complex healthcare services, directly impacting member satisfaction and the company's ability to execute its business strategy.
Centene's robust IT infrastructure, including advanced data analytics platforms, is fundamental to its operations. These systems manage vast amounts of member data, process millions of claims annually, and support critical care management initiatives. For instance, in 2023, Centene reported significant investments in technology to enhance its digital capabilities and data analytics, aiming to improve member engagement and health outcomes.
These sophisticated information technology systems are not just for operational efficiency; they are pivotal for understanding population health trends and informing strategic decisions. By leveraging data analytics, Centene can identify at-risk populations, personalize care plans, and optimize resource allocation. This data-driven approach allows the company to adapt to evolving healthcare landscapes and maintain a competitive edge.
Government Contracts and Licenses
Centene's business model heavily relies on government contracts and licenses, acting as a critical resource. These agreements, primarily for Medicaid, Medicare, and Health Insurance Marketplace programs, are the bedrock of its operations, allowing the company to serve millions of beneficiaries across various states.
These government partnerships are not merely operational permits; they represent significant revenue streams and market access. For instance, in 2024, Centene continued to leverage its extensive network of contracts to manage health benefits for a substantial portion of the US population eligible for government-sponsored healthcare programs.
- Medicaid Contracts: Centene holds numerous contracts with state governments to administer Medicaid benefits, providing managed care services to low-income individuals and families.
- Medicare Advantage Contracts: The company also secures contracts to offer Medicare Advantage plans, serving seniors and individuals with disabilities.
- Health Insurance Marketplace Agreements: Centene participates in state and federal Health Insurance Marketplaces, offering subsidized health plans to individuals and families.
- Regulatory Licenses: Essential operating licenses from state insurance departments and federal agencies are fundamental to conducting business in the healthcare sector.
Financial Capital
Centene requires substantial financial capital to manage its extensive operations, which include processing a high volume of healthcare claims and ensuring timely payments to providers. This capital is also crucial for investing in advanced technologies that streamline administrative processes and improve member care.
A robust financial foundation is paramount for Centene to maintain solvency and liquidity within the highly regulated and competitive managed healthcare sector. This allows the company to weather economic fluctuations and meet its ongoing obligations.
- Operational Funding: Centene's financial capital directly supports its day-to-day business, including claims processing and member services.
- Investment in Technology: Significant funds are allocated to technological advancements for efficiency and improved healthcare delivery.
- Strategic Growth: Capital enables Centene to pursue acquisitions and expand its market reach, as seen in its strategic moves. For instance, in 2023, Centene reported total revenue of $134.4 billion, underscoring the scale of its financial operations.
- Solvency and Liquidity: Maintaining a strong balance sheet is essential for Centene to remain a stable and reliable healthcare provider.
Centene's key resources include its vast provider networks, a large and skilled workforce, robust IT infrastructure, government contracts, and significant financial capital. These elements collectively enable the company to deliver comprehensive healthcare services, manage complex operations, and maintain a strong market position.
Value Propositions
Centene's value proposition centers on delivering affordable and comprehensive healthcare, particularly to those who are under-insured or uninsured. They achieve this by focusing on government-sponsored programs, effectively bridging the gap in access for vulnerable populations.
This approach directly tackles a significant societal need: ensuring individuals can receive quality medical care without facing prohibitive costs. For instance, in 2024, Centene's expansion into new markets aimed at increasing coverage for Medicaid and Medicare beneficiaries, underscoring their commitment to accessibility.
Centene's managed care programs are designed to directly enhance member health. In 2024, the company continued its focus on preventative screenings and chronic condition management, aiming to reduce hospital readmissions and improve quality of life for its diverse membership.
By integrating health services and addressing social determinants like housing and food security, Centene seeks to foster holistic well-being. This approach is crucial for vulnerable populations, contributing to better health outcomes beyond traditional medical care.
Centene provides budget-conscious healthcare strategies to state and federal governments overseeing Medicaid and Medicare. For instance, in 2023, Centene served approximately 15 million Medicaid members, demonstrating significant scale in managing these programs efficiently.
By focusing on proactive care and improving member health outcomes, Centene directly contributes to lowering the total cost of healthcare for its government partners. This approach helps governments achieve better value for taxpayer dollars.
Localized and Culturally Sensitive Care
Centene's commitment to localized and culturally sensitive care is a cornerstone of its value proposition, ensuring healthcare solutions resonate deeply within diverse communities. By tailoring services, the company fosters stronger member engagement and improved health outcomes.
This approach is crucial for building trust, as evidenced by Centene's significant presence in underserved areas. For instance, in 2023, Centene served approximately 16.4 million managed care members, with a substantial portion residing in rural and urban communities requiring tailored support.
- Community-Centric Approach: Centene prioritizes understanding and adapting to the unique cultural nuances and specific health needs of each community it serves.
- Enhanced Member Trust: This localized strategy cultivates deeper trust among members, leading to greater participation in health programs and adherence to care plans.
- Relevant Care Delivery: By embedding local insights, Centene delivers healthcare that is not only accessible but also culturally appropriate and highly relevant to members' lives.
Integrated Health Programs and Specialty Services
Centene offers a wide array of health programs and specialized services, consolidating care for its members. This includes crucial areas like behavioral health, pharmacy benefits management, and vision and dental care.
This integrated approach ensures members can access a comprehensive suite of necessary medical services conveniently. For instance, in 2024, Centene continued to expand its behavioral health offerings, recognizing the growing demand for mental health support.
- Integrated Care: Centene's model brings together diverse health services, simplifying access for members.
- Specialty Services: The company provides specialized care in areas such as behavioral health, pharmacy benefits, and vision/dental.
- Member Convenience: This consolidation aims to offer a one-stop solution for a broad range of healthcare needs.
- 2024 Focus: Continued expansion of behavioral health services highlights a key area of development.
Centene's value proposition is built on providing accessible, affordable, and comprehensive healthcare solutions, with a particular emphasis on government-sponsored programs like Medicaid and Medicare. This focus allows them to serve vulnerable populations effectively, bridging critical gaps in healthcare access. In 2024, Centene continued its strategic expansion to increase coverage for these beneficiaries, reinforcing its commitment to broad accessibility.
The company enhances member health through proactive and integrated care management, aiming to improve overall well-being and reduce healthcare costs. For instance, in 2024, Centene intensified its efforts in preventative care and chronic disease management to lower hospital readmissions and boost the quality of life for its members.
Centene also offers budget-conscious healthcare strategies to government entities, demonstrating efficiency in managing large-scale public health programs. In 2023, the company served approximately 15 million Medicaid members, showcasing its significant operational scale and ability to deliver value for taxpayer money by improving health outcomes.
A key differentiator is Centene's commitment to community-centric care, tailoring services to local needs and fostering trust. This localized approach, evident in their substantial presence in underserved areas, leads to greater member engagement and improved health outcomes. In 2023, Centene served around 16.4 million managed care members, many in areas requiring specialized support.
| Value Proposition Aspect | Description | Supporting Data/Focus (2023-2024) |
|---|---|---|
| Accessible & Affordable Healthcare | Bridging gaps for under-insured/uninsured via government programs. | Expansion into new markets for Medicaid/Medicare in 2024. |
| Enhanced Member Health Outcomes | Proactive care, chronic condition management, preventative services. | Focus on reducing hospital readmissions; expanding behavioral health in 2024. |
| Cost-Effective Government Solutions | Budget-conscious strategies for Medicaid/Medicare. | Managed approx. 15 million Medicaid members in 2023; improved health outcomes lower total costs. |
| Community-Centric & Integrated Care | Localized, culturally sensitive services; consolidated health programs. | Served ~16.4 million managed care members in 2023, many in underserved areas; expanded behavioral health. |
Customer Relationships
Centene excels in personalized member support, actively engaging individuals to understand their unique healthcare needs and navigate the complex system. This direct approach fosters trust and improves member satisfaction.
Through dedicated member services and targeted outreach, Centene aims to boost health literacy and ensure members can access the care they require. For instance, in 2023, Centene's proactive outreach programs contributed to a 15% increase in preventative care screenings among its Medicare Advantage members.
Centene actively builds trust and understanding by directly engaging with communities through outreach programs and health education. This hands-on approach allows them to grasp local health needs and ensure their services are both useful and easily accessible to the people they serve.
Centene’s business model heavily relies on fostering collaborative relationships with state and federal governments. This means maintaining open lines of communication and transparent reporting to ensure program compliance and success.
In 2024, Centene continued its focus on these partnerships, actively engaging with government agencies to adapt to evolving healthcare policies and regulations. This proactive approach is crucial for navigating the complexities of government-funded health programs.
The company's commitment to working closely with these entities directly impacts its ability to effectively serve its members and manage its contracts, which are often tied to government initiatives and funding streams.
Provider Relations and Support
Centene prioritizes robust provider relations, understanding that a well-supported network is crucial for delivering quality care. In 2024, the company continued to invest in resources and communication tools designed to streamline operations for its contracted healthcare providers. This focus directly impacts the efficiency of claims processing and the overall satisfaction of providers within Centene's extensive network.
Key aspects of Centene's provider support include:
- Dedicated Provider Support Teams: Offering accessible points of contact for inquiries and issue resolution.
- Educational Resources and Training: Providing materials to help providers navigate Centene's policies and procedures, including updates on reimbursement models.
- Timely Claims Processing: Aiming for efficient and accurate payment cycles to maintain provider financial health.
- Network Engagement Initiatives: Fostering collaboration through regular communication and feedback mechanisms to enhance the provider experience.
Digital Engagement and Self-Service Options
Centene is significantly boosting member convenience and engagement by leveraging digital platforms for self-service options, health information, and virtual care. This digital-first approach empowers members to manage their healthcare needs more independently.
- Digital Platforms: Centene's focus on digital engagement includes robust mobile apps and online portals, providing members with 24/7 access to their health plans.
- Self-Service Capabilities: Members can manage prescriptions, find providers, view claims, and update personal information directly through these digital channels, reducing reliance on call centers.
- Health Information & Virtual Care: The company offers extensive health resources and virtual care services, enabling members to access telehealth appointments and health education materials anytime, anywhere.
- Engagement Metrics: In 2024, Centene reported a notable increase in digital service utilization, with over 70% of member interactions occurring through digital channels, indicating strong adoption and satisfaction with these self-service options.
Centene cultivates strong relationships with both its members and healthcare providers through personalized engagement and robust support systems. By prioritizing direct communication and accessible resources, the company aims to enhance health literacy and ensure seamless care delivery.
In 2024, Centene continued to strengthen its government partnerships, focusing on transparent communication and compliance with evolving healthcare policies. This collaborative approach is fundamental to managing government-funded programs effectively.
Centene's commitment to digital transformation empowers members with self-service options and virtual care, increasing convenience and engagement. This digital-first strategy saw a significant rise in platform usage in 2024, with over 70% of member interactions occurring digitally.
| Relationship Type | Key Engagement Strategies | 2024 Focus/Impact |
|---|---|---|
| Member Relationships | Personalized support, digital platforms, health education | Increased digital service utilization (>70% of interactions), improved health literacy |
| Government Partnerships | Transparent communication, compliance reporting, policy adaptation | Navigating evolving healthcare regulations, ensuring program success |
| Provider Relationships | Dedicated support teams, educational resources, timely claims processing | Streamlined operations, enhanced provider satisfaction |
Channels
Centene primarily secures its business through direct contracts with state Medicaid agencies and the Centers for Medicare & Medicaid Services (CMS) for Medicare Advantage plans. These government bodies are the crucial conduits for Centene to serve eligible populations, representing its most significant distribution channels.
In 2024, Centene's extensive network of government contracts continued to be the bedrock of its revenue. For instance, the company's Medicaid business, a core component, consistently leverages these state-level agreements to expand its reach and service offerings across numerous states.
The Health Insurance Marketplace also serves as a vital channel, allowing Centene to offer plans to individuals and families who qualify for subsidies. This platform is essential for reaching a segment of the population not covered by traditional Medicaid or Medicare programs.
Centene leverages direct sales teams and a network of licensed insurance brokers to reach individuals and families for its Health Insurance Marketplace and Medicare Advantage plans. This dual approach ensures broad accessibility and personalized assistance during the crucial enrollment process.
In 2024, Centene's commitment to these channels is evident in its continued investment in sales force training and broker partnerships, aiming to simplify the complex process of selecting health coverage. These relationships are vital for guiding members through plan options and enrollment.
Centene leverages a vast network of hospitals, physician offices, clinics, and specialized facilities as its primary channel for delivering healthcare services. These established provider relationships are how members directly access the care they need. By the end of 2023, Centene managed care plans served approximately 27.5 million members, underscoring the scale of this network's reach.
Digital Platforms and Mobile Applications
Centene leverages its proprietary websites and mobile applications as key channels to connect with its members. These platforms facilitate crucial functions such as member enrollment, providing access to comprehensive health information, enabling users to locate healthcare providers, and offering convenient telemedicine services.
These digital tools significantly boost accessibility and user convenience, allowing members to manage their health needs efficiently. For instance, Centene’s mobile app offers features like prescription refills and appointment scheduling, streamlining the healthcare journey. In 2024, Centene reported a substantial increase in digital engagement, with millions of members actively using these platforms for various health management tasks.
- Member Enrollment: Streamlined online and app-based sign-ups.
- Health Information Access: Digital portals for benefits, claims, and wellness resources.
- Provider Finder: Tools to locate in-network doctors and facilities.
- Telemedicine Services: Virtual consultations for convenient healthcare access.
Community Outreach Programs and Local Offices
Centene leverages extensive community outreach programs and a network of local offices to connect with and serve under-insured and uninsured individuals. This strategy is crucial for building trust and providing accessible support directly within the communities they serve. For instance, in 2023, Centene reported significant investments in community health initiatives, aiming to address social determinants of health and improve member outcomes.
- Local Presence: Centene’s local offices act as vital touchpoints, offering in-person assistance for enrollment, benefits explanation, and care coordination.
- Community Engagement: Outreach programs, often conducted through partnerships with local organizations, focus on health education, preventative care, and addressing specific community needs.
- Trust Building: This direct, on-the-ground engagement fosters stronger relationships and greater trust among members, particularly those who may be hesitant to interact with traditional healthcare systems.
- Accessibility: By having a physical presence and actively engaging within communities, Centene enhances the accessibility of its services, ensuring that vulnerable populations can receive the support they need.
Centene's primary channels are its direct contracts with state Medicaid agencies and CMS for Medicare Advantage, which are the main avenues for serving eligible populations. The Health Insurance Marketplace is another key channel for individuals and families, particularly those receiving subsidies.
Centene also utilizes direct sales teams and brokers to reach individuals for its Marketplace and Medicare Advantage plans, simplifying the enrollment process.
Its digital platforms, including websites and mobile apps, are crucial for member engagement, offering enrollment, health information, provider locators, and telemedicine.
Community outreach and local offices are vital for connecting with under-insured and uninsured populations, building trust and providing accessible support.
Customer Segments
Medicaid beneficiaries represent a core customer segment for Centene, encompassing low-income individuals and families, pregnant women, children, and individuals with disabilities who qualify for government-funded healthcare. Centene's extensive experience and market presence make it a leading provider for these often vulnerable populations.
In 2024, Centene continued to serve millions of Medicaid members, demonstrating its significant reach within this demographic. The company's business model is heavily reliant on its ability to effectively manage care and costs for these individuals, often through managed care contracts with state governments.
Centene's Medicare beneficiaries, encompassing seniors and individuals with disabilities, represent a crucial customer segment. Through its Wellcare brand, Centene provides Medicare Advantage (Part C) and Prescription Drug Plans (PDPs), often targeting those with lower incomes and more complex health requirements.
In 2024, Centene's Medicare segment continued to be a significant driver of its business, with the company serving millions of Medicare members. This segment is characterized by a growing population of eligible individuals and a strong demand for comprehensive health coverage, including prescription drug benefits.
Centene's Health Insurance Marketplace enrollees are individuals and families who need health coverage but don't qualify for government programs like Medicaid or Medicare. These are the people utilizing the Affordable Care Act (ACA) marketplace to find affordable plans. Centene's Ambetter Health brand is a key player here, offering a range of options to this demographic.
In 2024, the ACA marketplace continued to be a vital source of coverage. For instance, during the 2024 open enrollment period, which ran from November 1, 2023, to January 16, 2024, a significant number of Americans selected plans. The Centers for Medicare & Medicaid Services (CMS) reported that over 21 million Americans enrolled in a Health Insurance Marketplace plan for 2024 coverage, demonstrating the ongoing demand for these services.
Dual-Eligible Individuals (Medicaid and Medicare)
Dual-eligible individuals, those qualifying for both Medicare and Medicaid, represent a particularly intricate customer segment for Centene. These individuals often have complex health needs and require coordinated care across different benefit systems.
Centene addresses this segment through specialized products like Dual Eligible Special Needs Plans (D-SNPs). These plans are designed to integrate the benefits and services provided by both Medicare and Medicaid, aiming for a more seamless and effective healthcare experience for the member.
- Targeting Dual-Eligibles: Centene focuses on individuals eligible for both Medicare and Medicaid, a group with significant healthcare needs.
- Specialized Plans: The company offers Dual Eligible Special Needs Plans (D-SNPs) to cater to this specific population.
- Integrated Care: D-SNPs aim to provide a unified approach to care, combining Medicare and Medicaid benefits.
- Market Presence: As of early 2024, Centene is a significant player in the D-SNP market, managing millions of dual-eligible members across various states.
Under-insured and Uninsured Individuals
Centene's core customer base comprises individuals who are either under-insured or have no insurance coverage at all. This segment is characterized by a substantial need for healthcare services, often relying on government-sponsored programs for their medical care.
In 2024, the number of uninsured individuals in the United States remained a significant concern, with estimates suggesting millions still lacked adequate health coverage. Centene actively targets these populations, understanding their reliance on programs like Medicaid and Medicare. This focus allows them to provide essential health benefits to those who would otherwise struggle to access care.
The company's business model is built around managing the complexities of these government programs, ensuring that under-insured and uninsured individuals receive the necessary medical attention. This approach addresses a critical gap in the healthcare market.
- Significant Market: Millions of Americans lack adequate health insurance, creating a large addressable market for Centene.
- Government Program Focus: Centene specializes in serving beneficiaries of government-sponsored healthcare, including Medicaid and Medicare.
- Access to Care: By enrolling these individuals, Centene facilitates their access to vital healthcare services and treatments.
- Health Needs: This demographic often has higher healthcare utilization rates, requiring comprehensive and managed care solutions.
Centene's customer segments are primarily defined by their eligibility for government-sponsored health insurance programs. This includes Medicaid beneficiaries, who are low-income individuals and families, and Medicare beneficiaries, consisting of seniors and individuals with disabilities. The company also serves individuals purchasing coverage through the Health Insurance Marketplace, often referred to as ACA enrollees, and a crucial, complex group known as dual-eligible individuals who qualify for both Medicare and Medicaid.
In 2024, Centene continued to manage a vast number of members across these segments. For example, the company reported serving approximately 17.5 million Medicaid members and over 4.4 million Medicare members as of the first quarter of 2024, underscoring its significant market penetration in these government-funded healthcare areas.
The Health Insurance Marketplace, particularly through its Ambetter Health brand, remains a key area for Centene. The 2024 open enrollment period saw robust participation, with over 21 million Americans selecting plans for 2024 coverage, indicating a sustained demand for affordable healthcare options outside of traditional government programs.
Centene's strategic focus on these diverse, often underserved, populations allows it to leverage its expertise in managed care to provide essential health services. The company's ability to navigate the complexities of these different customer segments and their associated regulatory frameworks is central to its business model.
Cost Structure
The Health Benefits Ratio (HBR) is the most significant element within Centene's cost structure, reflecting the direct expenses incurred for healthcare services provided to its members. This ratio encompasses a broad range of expenditures, including payments to providers for doctor visits, hospitalizations, prescription medications, and various other medical treatments.
In 2024, Centene's HBR was approximately 88.3%, indicating that nearly 89 cents of every premium dollar was spent on healthcare. This figure highlights the critical nature of managing medical costs, as even minor shifts in member health needs or how often they access care can have a substantial effect on profitability.
Selling, General, and Administrative (SG&A) expenses at Centene encompass critical operational costs including employee salaries, marketing campaigns, technology investments, and general administrative overhead. These costs are fundamental to running the business day-to-day and supporting its growth.
Centene has actively pursued strategies to optimize its SG&A expenses, recognizing the impact on profitability. A key focus has been on efficiency initiatives designed to streamline operations and reduce waste. Leveraging its significant scale as a major managed care provider allows Centene to negotiate better terms for services and technology, thereby lowering per-member costs.
For the first quarter of 2024, Centene reported SG&A expenses of $2.3 billion. This represents a notable increase from the $2.1 billion reported in the first quarter of 2023, reflecting investments in growth initiatives and ongoing operational adjustments.
Centene's cost structure heavily features provider payments and network management. These expenses encompass direct payments to a vast array of healthcare providers, including hospitals and physicians, essential for delivering care to its members. For instance, in 2023, Centene's cost of care, which largely reflects these provider payments, was approximately $122.5 billion.
Furthermore, managing and expanding its extensive provider network involves significant operational costs. This includes the resources dedicated to establishing and maintaining relationships, ensuring network adequacy, and implementing quality initiatives. The company's investment in value-based care arrangements, aimed at improving patient outcomes and controlling costs, also adds to these network management expenses.
Technology and Infrastructure Investments
Centene makes substantial ongoing investments in its technology and infrastructure. These are not one-off expenses but rather continuous outlays essential for staying competitive and compliant in the healthcare sector.
These significant investments are channeled into critical areas such as advanced information technology systems, robust data analytics capabilities, and sophisticated digital health platforms. For instance, in 2023, Centene reported technology and development expenses of approximately $1.5 billion, a testament to the scale of these commitments.
- Information Technology Systems: Upgrades and maintenance of core IT infrastructure, including cloud services and network security, are paramount.
- Data Analytics Capabilities: Investment in tools and personnel to analyze vast amounts of health data for better member outcomes and operational insights.
- Digital Health Platforms: Development and enhancement of member-facing apps, telehealth services, and provider portals to improve engagement and access.
- Operational Efficiency & Security: These investments directly support streamlined operations, data protection, and regulatory compliance, ensuring member trust and system integrity.
Regulatory Compliance and Legal Costs
Centene faces significant expenses to maintain compliance with the complex web of healthcare regulations. This includes costs for legal counsel, regulatory filings, and ongoing monitoring to ensure adherence to laws like the Affordable Care Act and HIPAA. For instance, in 2023, the healthcare industry as a whole saw substantial spending on compliance, with estimates suggesting companies allocate a significant portion of their operating budget to these efforts.
These regulatory compliance and legal costs are critical for Centene’s operations. They encompass various activities:
- Licensing and Accreditation: Securing and maintaining necessary licenses in each state of operation, along with accreditation from bodies like NCQA.
- Legal Counsel and Defense: Engaging legal experts to navigate regulatory changes, respond to inquiries, and defend against potential litigation or government investigations.
- Compliance Monitoring and Auditing: Implementing systems and processes to track adherence to regulations and conducting internal audits to identify and rectify any non-compliance issues.
- Policy Development and Training: Creating and updating internal policies and providing regular training to employees on regulatory requirements.
Centene's cost structure is dominated by the Health Benefits Ratio (HBR), which represented about 88.3% of premium dollars in 2024, highlighting the direct cost of healthcare services. Selling, General, and Administrative (SG&A) expenses, including salaries and technology, were $2.3 billion in Q1 2024, up from $2.1 billion in Q1 2023, indicating investment in growth. Provider payments, a core component of the cost of care, reached approximately $122.5 billion in 2023, underscoring the significant outlay for healthcare delivery.
| Cost Category | 2023 (Approximate) | Q1 2024 (Approximate) | Significance |
|---|---|---|---|
| Health Benefits Ratio (HBR) | N/A | 88.3% of premiums | Direct cost of healthcare services |
| Cost of Care (primarily provider payments) | $122.5 billion | N/A | Payments to hospitals, physicians, etc. |
| SG&A Expenses | N/A | $2.3 billion | Operational costs, marketing, technology |
| Technology & Development | $1.5 billion | N/A | IT systems, data analytics, digital platforms |
Revenue Streams
Centene's core revenue generation hinges on premiums collected for its government-sponsored health plans. This includes significant income from Medicaid, Medicare Advantage, Medicare Prescription Drug Plans, and plans offered through the Health Insurance Marketplace.
These premiums are primarily sourced from government entities, both state and federal, with additional contributions coming from members who benefit from subsidies. For instance, in 2024, Centene's revenue from these government programs is projected to be substantial, reflecting the vast number of individuals enrolled in their plans across various states and federal initiatives.
Centene's revenue streams prominently feature risk adjustment payments within the Health Insurance Marketplace. These payments are crucial, acting as compensation for health plans that enroll members with higher healthcare needs, often referred to as sicker members. This mechanism helps to level the playing field among insurers.
For 2024, these risk adjustment payments represent a substantial portion of Centene's overall revenue. While specific figures fluctuate based on the aggregated health status of their enrolled population and evolving government methodologies, Centene has historically relied on these payments to support its business model, particularly in the government-sponsored health plan sector.
Centene's revenue is also bolstered by its specialty services. These can encompass a range of offerings like pharmacy benefit management (PBM), which helps manage prescription drug benefits for health plans, and behavioral health services, addressing mental and emotional well-being. In 2023, Centene reported significant revenue from these diversified services, contributing to their overall financial performance.
Investment Income
Centene generates investment income from its substantial cash reserves and its diverse investment portfolio. This income, while often a smaller portion of its total revenue compared to premium collections, plays a role in bolstering the company's financial performance.
For instance, in the first quarter of 2024, Centene reported investment and other income of $250 million. This demonstrates the tangible contribution of its investment activities to the company's bottom line.
- Investment Income Contribution: Centene's investment income, derived from managing its cash and securities, adds to its overall revenue stream.
- Q1 2024 Performance: In the first three months of 2024, Centene saw $250 million in investment and other income.
- Portfolio Management: The effective management of its investment portfolio is key to maximizing returns from these assets.
Other Contractual Revenue and Fees
Centene's revenue streams extend beyond direct health plan premiums to include fees generated from administrative services for self-funded employer plans. These arrangements often involve managing claims, processing payments, and providing other operational support, creating a steady income stream. For instance, in 2023, Centene reported significant revenue from these types of contractual services, contributing to their overall financial performance.
These contractual arrangements can also encompass partnerships with various healthcare organizations, where Centene might offer specialized services or share in revenue generated from joint ventures. Such diversification in revenue sources helps to stabilize earnings and reduce reliance on a single business line. In the first quarter of 2024, the company continued to leverage these diverse contractual relationships to bolster its financial results.
- Administrative Service Fees: Revenue from managing self-funded health plans for employers.
- Contractual Arrangements: Income derived from partnerships and agreements with other healthcare entities.
- Ancillary Services: Fees for specialized services offered to members or providers.
Centene's revenue is primarily built on premiums from government health plans like Medicaid and Medicare Advantage. Additional income comes from risk adjustment payments, which compensate for enrolling members with higher healthcare needs. The company also generates revenue from specialty services such as pharmacy benefit management and behavioral health, alongside investment income from its reserves.
| Revenue Stream | Description | 2024 Projection/Contribution |
|---|---|---|
| Government Health Plan Premiums | Premiums from Medicaid, Medicare Advantage, Medicare PDPs, and Marketplace plans. | Primary revenue driver, substantial portion of total revenue. |
| Risk Adjustment Payments | Compensation for enrolling members with higher healthcare needs. | Significant contributor, especially within the Health Insurance Marketplace. |
| Specialty Services | Pharmacy benefit management (PBM), behavioral health services, etc. | Contributed significantly to financial performance in 2023. |
| Investment Income | Income from cash reserves and investment portfolio. | Q1 2024: $250 million in investment and other income. |
| Administrative Service Fees & Contractual Arrangements | Fees for managing self-funded plans and revenue from partnerships. | Steady income stream from contractual services and joint ventures. |
Business Model Canvas Data Sources
The Centene Business Model Canvas is built using a combination of internal financial data, extensive market research on healthcare trends, and competitive analysis of other managed care organizations. These diverse data sources ensure each component of the canvas is grounded in empirical evidence and strategic understanding.
