agilon health PESTLE Analysis
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
agilon health Bundle
Uncover the external forces shaping agilon health's trajectory with our comprehensive PESTLE analysis. From evolving political landscapes impacting healthcare policy to economic shifts influencing patient access and technological advancements in value-based care, we dissect every critical factor. Understand the social trends driving demand for integrated health solutions and the environmental considerations within the healthcare sector. Don't be left guessing about what's next; gain a competitive advantage by downloading our full, actionable PESTLE analysis today and unlock strategic foresight.
Political factors
Government policies, particularly from the Centers for Medicare & Medicaid Services (CMS), are a significant driver for Agilon Health's value-based care model. CMS initiatives continue to push for better patient outcomes and cost control within Medicare and Medicare Advantage. For instance, the CMS's Medicare Shared Savings Program (MSSP) saw a significant increase in participating ACOs, with over 600 ACOs participating in 2023, demonstrating the ongoing commitment to value-based payment models.
Agilon Health's success is directly linked to the ongoing stability and growth of these governmental programs. While specific program details or risk adjustments may evolve, the fundamental direction from CMS remains focused on value. For 2024, CMS projected continued growth in Medicare Advantage enrollment, which directly expands the pool of beneficiaries in value-based arrangements that Agilon Health can serve.
Changes in Medicare Advantage (MA) regulations and payment rates directly affect Agilon Health's business model, which centers on value-based care for seniors. The Centers for Medicare & Medicaid Services (CMS) frequently revises MA policies, influencing payment rates, Star Ratings, and required benefits, all of which can alter partner plan offerings and financial sustainability.
For example, the CMS announced an overall payment increase for MA plans in 2025. However, adjustments to risk adjustment models and supplemental benefits are also key considerations, potentially reshaping plan designs and influencing Agilon's strategic operational planning.
Broader healthcare reform initiatives beyond value-based care can significantly impact Agilon Health. Policies influencing affordability, access, and quality are shaping the market landscape, presenting both opportunities and potential hurdles.
The Inflation Reduction Act of 2022, for instance, introduced measures designed to lower prescription drug costs. While its aim is to benefit patients, such as through the $2,000 out-of-pocket cap for Medicare Part D beneficiaries starting in 2025, these changes necessitate strategic adjustments from healthcare providers and their partners like Agilon Health.
These reforms can alter patient behavior, provider reimbursement models, and the competitive environment. Agilon Health must navigate these evolving regulations to maintain its growth trajectory and effectively serve its partner physician groups.
Regulatory Scrutiny and Enforcement
Agilon Health operates within a highly regulated healthcare landscape, facing increasing scrutiny. Recent enforcement actions highlight a heightened focus on data privacy under HIPAA and anti-fraud measures within Medicare Advantage plans. For instance, the U.S. Department of Justice has been actively pursuing healthcare providers for alleged fraudulent billing practices, with significant settlements occurring throughout 2024.
Navigating these complex federal and state regulations presents a continuous compliance challenge for Agilon. The company must ensure its technology platforms and service delivery models align with evolving standards in areas like risk adjustment and quality reporting. Failure to do so could result in substantial financial penalties and damage to its reputation.
- Increased government oversight on healthcare data privacy and security measures.
- Focus on preventing fraud, waste, and abuse within government healthcare programs.
- Potential for significant fines and legal repercussions for non-compliance with regulations like the False Claims Act.
- Agilon's need to adapt its operational and technological frameworks to meet evolving compliance requirements.
Political Stability and Healthcare Spending Priorities
The political landscape significantly shapes healthcare policy, directly impacting agilon health's operational environment. Federal budget priorities, often debated in Congress, determine the allocation of funds for programs like Medicare and Medicaid, which are crucial for agilon's value-based care models. For instance, the Medicare Advantage program, a key area for agilon, saw continued growth, with enrollment projected to reach over 33 million beneficiaries in 2024, representing a substantial market for their services.
While there's a general consensus across both major parties regarding the benefits of shifting towards value-based care, specific implementation details and funding levels can fluctuate with changes in administration or economic pressures. For example, the Biden administration has continued to emphasize value-based care initiatives, aiming to increase the number of Americans in such arrangements. However, potential shifts in congressional control could alter the legislative agenda and the pace of these reforms.
Agilon Health must remain agile, ready to adjust its strategies in response to evolving government healthcare spending priorities. The Centers for Medicare & Medicaid Services (CMS) regularly updates payment models and quality metrics, requiring continuous adaptation. The Inflation Reduction Act of 2022, for instance, included provisions that could impact drug pricing and Medicare spending, necessitating careful monitoring by companies like agilon.
- Federal Budget Impact: The annual federal budget process dictates funding for Centers for Medicare & Medicaid Services (CMS) programs, directly affecting reimbursement rates and the viability of value-based care models.
- Bipartisan Support for Value-Based Care: Despite political shifts, there's a sustained, albeit varied, commitment to value-based payment models across the political spectrum, offering a degree of stability for agilon's core strategy.
- Medicare Advantage Growth: Continued enrollment increases in Medicare Advantage plans, projected to exceed 33 million in 2024, highlight the expanding market opportunity for agilon's integrated care solutions.
- Policy Adaptability: Agilon needs to proactively adapt to potential legislative changes, such as those related to drug pricing or Medicare spending limits, to maintain its competitive edge.
Government policies, particularly those from the Centers for Medicare & Medicaid Services (CMS), significantly influence Agilon Health's value-based care model. The ongoing push for better patient outcomes and cost control within Medicare and Medicare Advantage programs directly impacts Agilon's operational framework. For instance, Medicare Advantage enrollment continued its upward trend, with projections indicating over 33 million beneficiaries in 2024, expanding the market Agilon serves.
CMS's evolving regulations for Medicare Advantage plans, including payment rates and risk adjustment models, are critical. For 2025, CMS announced an overall payment increase for MA plans, but adjustments to risk adjustment and supplemental benefits require continuous strategic planning by Agilon. Broader healthcare reforms, like the Inflation Reduction Act's measures on prescription drug costs, also necessitate adaptation, such as the $2,000 out-of-pocket cap for Medicare Part D beneficiaries starting in 2025.
Increased government oversight on data privacy and fraud prevention within Medicare Advantage plans presents ongoing compliance challenges. Agilon must ensure its technology and service delivery models align with evolving standards in areas like risk adjustment and quality reporting to avoid penalties. For example, the U.S. Department of Justice's active pursuit of healthcare providers for alleged fraudulent billing throughout 2024 underscores the importance of robust compliance measures.
The political landscape, including federal budget priorities and legislative agendas, directly affects funding for CMS programs. While there's bipartisan support for value-based care, specific implementation and funding levels can shift. Agilon must remain agile to adapt to potential legislative changes and evolving government healthcare spending priorities to maintain its growth trajectory.
What is included in the product
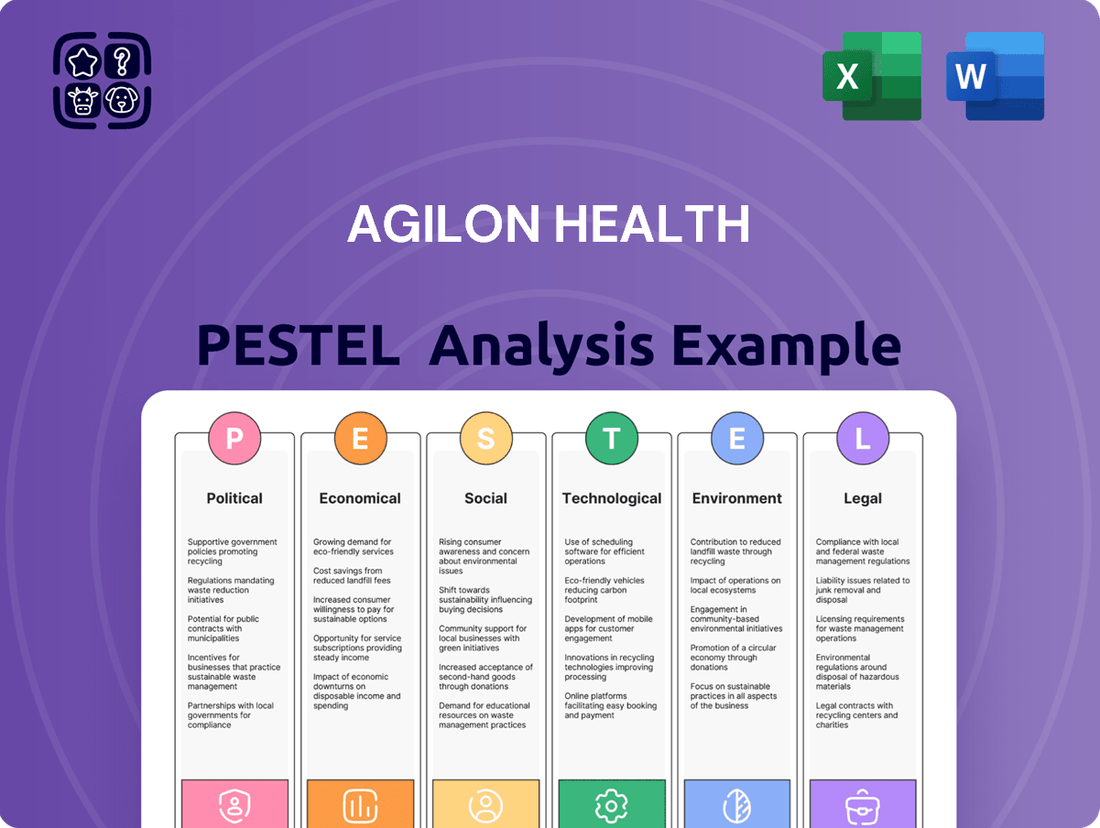
This PESTLE analysis delves into the Political, Economic, Social, Technological, Environmental, and Legal forces shaping agilon health's operational landscape, providing a comprehensive overview of external influences.
It offers actionable insights by highlighting key trends and potential impacts, empowering strategic decision-making for agilon health in the dynamic healthcare sector.
The agilon health PESTLE Analysis serves as a pain point reliever by providing a structured framework to identify and navigate external factors impacting value-based care, enabling proactive strategy development.
It simplifies complex market dynamics, offering a clear, actionable overview of political, economic, social, technological, environmental, and legal influences to alleviate the pain of uncertainty in healthcare planning.
Economic factors
The persistent upward trend in national healthcare expenditures, including employer-sponsored plans, strongly favors value-based care. This economic reality creates a significant incentive for innovative models like agilon health's.
Forecasts suggest healthcare spending will continue to outpace overall GDP growth. For instance, U.S. healthcare spending was projected to reach $7.0 trillion by 2031, growing at an average annual rate of 5.4% according to CMS projections. This persistent cost escalation makes effective cost control a paramount objective for both insurance payers and healthcare providers.
Agilon Health's model is strategically designed to tackle this economic headwind by focusing on reducing overall healthcare costs through enhanced patient outcomes. Their approach directly addresses the financial pressures faced by the healthcare system.
The healthcare industry's shift from fee-for-service (FFS) to value-based care (VBC) is a significant economic factor for Agilon Health. This transition rewards providers for patient outcomes and quality of care, not just the number of services rendered, which directly supports Agilon's model. For instance, Medicare’s shift towards VBC, with initiatives like the ACO REACH model, indicates a growing market for Agilon's platform.
Agilon Health's revenue and growth are intrinsically linked to the success and expansion of these risk-based payment models. As more healthcare systems embrace VBC, the demand for Agilon's capabilities in managing populations under these arrangements increases. The Centers for Medicare & Medicaid Services (CMS) continues to push VBC, with reports suggesting a substantial portion of Medicare payments are already tied to quality and value by 2024 and projected to grow further.
Healthcare providers and payers are feeling the pinch from escalating operational expenses, a persistent lack of skilled staff, and, in some instances, reduced reimbursement rates. This economic squeeze amplifies the appeal of collaborations with entities like Agilon Health, which offer crucial capital, advanced technology, and specialized services designed to navigate risk and boost operational effectiveness.
The financial strain on the healthcare sector is palpable. For example, the average hospital operating margin was projected to be around 3.2% in 2024, a tight figure that leaves little room for error amidst rising costs. This environment makes Agilon's model, which supports physician groups in maintaining their autonomy while excelling within value-based care frameworks, a particularly compelling proposition.
Economic Downturns and Market Volatility
Economic downturns and market volatility pose significant risks to agilon health's operational and financial stability. A contraction in the economy can directly affect healthcare spending, leading to reduced patient enrollment in insurance plans and potentially straining the financial health of the physician groups agilon partners with. For instance, during periods of economic stress, discretionary healthcare spending often declines, impacting patient access to services.
While the healthcare sector is often seen as defensive, severe economic contractions can still exert pressure. Government budgets allocated to Medicare and Medicaid, crucial for agilon’s model, could face cutbacks, affecting reimbursement rates. Similarly, individuals may struggle with out-of-pocket expenses for supplemental benefits, impacting their ability to maintain coverage.
Agilon Health's financial performance, specifically its revenue streams and medical margins, is susceptible to these macroeconomic shifts. For example, in the first quarter of 2024, U.S. GDP growth slowed to an annualized rate of 1.3%, indicating a cooling economy that could translate into tighter consumer budgets and increased pressure on healthcare providers.
- Impact on Healthcare Spending: Economic slowdowns can lead to reduced consumer spending on non-essential medical services and a greater reliance on government-funded programs.
- Government Budgetary Pressures: A weaker economy may force governments to re-evaluate spending on healthcare programs like Medicare and Medicaid, potentially impacting reimbursement levels for providers.
- Patient Affordability: Market volatility and job losses associated with economic downturns can diminish patients' ability to afford supplemental insurance or pay for healthcare services not fully covered by primary plans.
- Physician Group Financial Health: Partnered physician groups may experience decreased patient volumes and cash flow issues during economic contractions, affecting their ability to invest in value-based care models.
Competition in the Value-Based Care Market
The value-based care (VBC) market is seeing a surge in competition, with payer-owned practices and other VBC enablers actively entering the arena. This intensified rivalry puts pressure on companies like agilon health to clearly articulate their unique value proposition and partnership approach to draw in and keep physician groups. For instance, in 2024, many large insurance providers are expanding their direct care models, aiming to capture more of the VBC market share.
This escalating competition directly impacts pricing strategies and the breadth of services offered. Agilon Health will need to continually innovate its platform to maintain its competitive edge. Market analysis for 2024 indicates a trend towards integrated solutions that offer more than just administrative support, pushing all players to enhance their technological capabilities and patient engagement strategies.
- Increased Payer Involvement: Major health insurers are launching or acquiring physician groups to directly manage VBC arrangements, adding significant competition.
- Emergence of VBC Enablers: New technology platforms and consulting firms are offering VBC solutions, fragmenting the market and increasing partnership choices for providers.
- Focus on Differentiation: Agilon Health's success hinges on demonstrating superior outcomes, cost savings, and physician satisfaction compared to emerging competitors.
- Impact on Physician Groups: Physician groups now have more options, necessitating attractive partnership terms and demonstrable value from VBC enablers.
The healthcare industry's ongoing shift towards value-based care (VBC) presents a significant economic tailwind for Agilon Health. As payers increasingly prioritize outcomes over volume, Agilon's model, designed to manage populations under risk-based arrangements, becomes more attractive. For instance, by the end of 2023, over 60% of Medicare payments were already tied to value, a trend expected to accelerate.
Escalating healthcare costs continue to drive demand for cost-effective solutions. U.S. healthcare spending was projected to reach approximately $7.0 trillion by 2031, with CMS forecasting an average annual growth rate of 5.4%. Agilon's ability to improve patient outcomes and manage total cost of care directly addresses this economic pressure for providers and payers alike.
Physician groups are experiencing financial strain due to rising operational expenses and workforce shortages, making partnerships like those offered by Agilon Health appealing. With average hospital operating margins hovering around 3.2% in 2024, efficiency and cost management are critical, and Agilon provides the capital and expertise to navigate these challenges.
Economic downturns pose a risk, potentially impacting healthcare spending and government budgets for programs like Medicare and Medicaid. A cooling economy, as indicated by a 1.3% annualized GDP growth in Q1 2024, could lead to reduced patient volumes and tighter budgets for healthcare providers, affecting Agilon's revenue streams.
| Economic Factor | Impact on Agilon Health | Supporting Data (2024/2025 Projections) |
|---|---|---|
| Value-Based Care (VBC) Growth | Increased demand for Agilon's population health management platform. | Over 60% of Medicare payments linked to value by end of 2023; projected to increase. |
| Healthcare Spending Escalation | Drives need for cost-control solutions like Agilon's model. | U.S. healthcare spending projected at $7.0 trillion by 2031 (5.4% annual growth). |
| Provider Financial Strain | Enhances appeal of Agilon's capital and operational support. | Average hospital operating margins around 3.2% in 2024. |
| Economic Slowdown Risk | Potential reduction in healthcare spending and government program funding. | Q1 2024 U.S. GDP growth at 1.3%; indicates potential for tighter consumer budgets. |
Full Version Awaits
agilon health PESTLE Analysis
The preview shown here is the exact document you’ll receive after purchase—fully formatted and ready to use. This comprehensive PESTLE analysis of Agilon Health delves into the Political, Economic, Social, Technological, Legal, and Environmental factors influencing its operations. Understand the market dynamics, regulatory landscape, and societal trends impacting the company's strategic decisions and future growth. This in-depth report provides actionable insights for stakeholders navigating the healthcare sector.
Sociological factors
The growing number of older adults, particularly those over 65, is a significant societal shift. By 2030, the U.S. Census Bureau projects that this age group will represent over 20% of the total population, a substantial increase from around 16% in 2020. This demographic is precisely agilon health's core focus, meaning a larger pool of potential patients seeking their specialized care model.
This aging demographic is also more likely to experience multiple chronic diseases, often referred to as multimorbidity. For instance, data from the Centers for Disease Control and Prevention (CDC) indicates that over 60% of adults aged 65 and older have at least two chronic conditions, such as diabetes, heart disease, or arthritis. This reality underscores the need for healthcare solutions that go beyond treating individual ailments to managing overall patient health proactively.
Agilon health's model is designed to address this very challenge. By concentrating on value-based care for seniors, they aim to improve health outcomes and reduce costs associated with managing complex, chronic conditions. Their success is directly tied to their ability to navigate the healthcare needs of this expanding and often sicker population segment, making this trend a fundamental driver of their business.
Patients, particularly seniors, are increasingly demanding healthcare that feels more seamless and personalized, focusing on their unique needs and holistic health. This shift in preference means providers need to offer care that's not just reactive but proactive and integrated across different services.
Agilon Health's strategy directly addresses this by enabling doctors to provide this type of patient-focused care, aiming to boost health outcomes. For instance, a significant portion of seniors, often over 65, are looking for better chronic condition management, which coordinated care facilitates.
The growing importance of patient engagement tools and the expansion of home-based care options are key indicators of this trend. By 2024, studies show that patient satisfaction scores are directly linked to the accessibility and coordination of their care plans, with many preferring to manage their health from the comfort of their homes.
Societal emphasis on health equity and Social Determinants of Health (SDOH) significantly shapes healthcare. For instance, a 2024 report highlighted that individuals from lower socioeconomic backgrounds experience higher rates of chronic diseases, underscoring the need for SDOH interventions. This trend directly impacts how healthcare is delivered and regulated.
Value-based care models are now incorporating financial incentives designed to tackle health disparities and fund SDOH initiatives. By 2025, Medicare Advantage plans are projected to allocate substantial resources towards addressing factors like food insecurity and transportation access, a shift driven by these new reimbursement structures.
Agilon Health's strategic partnerships are crucial for leveraging data and community ties. These collaborations allow them to better meet the comprehensive needs of their patient populations. For example, by partnering with local food banks, agilon can directly improve nutritional outcomes for at-risk seniors, thereby advancing health equity.
Physician Burnout and Workforce Shortages
The healthcare sector, a key area for agilon health, is grappling with severe physician burnout and critical workforce shortages, especially in primary care. This trend impacts patient access and quality of care across the nation.
Agilon Health's model directly addresses these sociological challenges by streamlining administrative tasks and boosting clinical efficiency for physicians. This allows practitioners to dedicate more time to patient interaction, a crucial factor in combating burnout.
By enabling physicians to maintain practice independence and focus on patient well-being, agilon health's platform fosters a more sustainable and fulfilling career path. This approach is vital for retaining experienced physicians and attracting new talent to the field.
- Physician burnout rates remain alarmingly high, with studies indicating over 50% of physicians experiencing symptoms.
- A projected shortage of up to 124,000 physicians by 2034 in the U.S. underscores the urgency of addressing workforce issues.
- Agilon Health's platform aims to alleviate administrative burdens, which are cited as a major contributor to physician dissatisfaction.
Public Trust and Transparency in Healthcare
Public trust in the healthcare sector has seen a notable decline, with a 2023 Gallup poll indicating that only 31% of Americans have high confidence in the healthcare system. This erosion of trust is largely fueled by persistent concerns about the affordability and transparency of medical services. Agilon Health's focus on value-based care, which prioritizes patient outcomes and cost efficiency, directly addresses these public anxieties. By demonstrating clear improvements in health results and a reduction in overall spending, Agilon can foster a more positive perception among patients and communities. The company's strategy to enhance transparency, particularly around pricing and service costs, is crucial for rebuilding confidence.
Agilon Health's model is designed to align incentives, rewarding providers for keeping patients healthy and managing costs effectively. This approach is particularly relevant as healthcare spending continues to be a major concern; in 2024, healthcare costs are projected to be a significant burden for many households. Transparency in billing and clear communication about expected expenses are paramount for patients navigating these costs. Agilon's commitment to these principles supports a more patient-centric model that can help restore faith in the system.
Key aspects influencing public trust include:
- Patient-centricity: Shifting focus from volume of services to quality of care and patient well-being.
- Affordability: Addressing the rising cost of healthcare and ensuring accessible services.
- Transparency: Providing clear information on pricing, treatment options, and expected outcomes.
- Outcome-driven care: Demonstrating measurable improvements in patient health and satisfaction.
The aging U.S. population is a foundational sociological factor for agilon health, with individuals over 65 projected to be over 20% of the population by 2030. This demographic often faces multiple chronic conditions, with over 60% of those aged 65+ having at least two such ailments, as reported by the CDC. Agilon's value-based care model directly addresses the needs of this expanding, complex patient base by focusing on proactive, coordinated health management.
Societal demands for more personalized and seamless healthcare experiences are also crucial. Patients increasingly prefer integrated care plans and home-based options, with satisfaction linked to accessibility. Agilon's strategy empowers physicians to deliver this patient-focused approach, enhancing chronic condition management for seniors seeking coordinated care.
Furthermore, a growing emphasis on health equity and Social Determinants of Health (SDOH) is reshaping healthcare delivery. Reports in 2024 indicate higher chronic disease rates in lower socioeconomic groups, prompting value-based care models to incorporate SDOH initiatives and address factors like food insecurity and transportation access, often through strategic partnerships.
Physician burnout, impacting over 50% of practitioners, and projected physician shortages, potentially reaching 124,000 by 2034, are significant challenges. Agilon Health's model aims to mitigate this by reducing administrative burdens, allowing physicians more time for patient care and fostering practice independence, thereby improving career sustainability.
Declining public trust in healthcare, with only 31% of Americans expressing high confidence in 2023, is another key factor. Agilon's focus on patient-centricity, affordability, transparency, and outcome-driven care directly tackles these concerns, aiming to rebuild confidence through improved health results and cost efficiency.
Technological factors
The rapid advancements in data analytics and AI are fundamentally reshaping how Agilon Health manages its patient populations. These technologies are vital for identifying individuals at higher risk, allowing for proactive interventions. For example, by 2025, the healthcare analytics market is projected to reach $59.1 billion globally, highlighting the increasing reliance on these tools.
AI-powered solutions offer Agilon Health the capability to optimize resource allocation, ensuring that care is delivered where and when it's most needed. This leads to more personalized patient interventions and a significant streamlining of administrative processes, ultimately boosting the efficiency and effectiveness of their value-based care models. Agilon's strategic partnerships with AI firms underscore their commitment to leveraging these capabilities.
The increasing integration of telehealth and remote patient monitoring (RPM) is a significant technological factor reshaping healthcare. These tools allow for continuous patient oversight and convenient access to care, especially beneficial for managing chronic conditions in older adults. By 2024, the global telehealth market was projected to reach over $200 billion, highlighting its rapid expansion. Agilon Health's model is well-positioned to harness these advancements, extending its reach and enhancing patient engagement through virtual consultations and remote data collection, thereby potentially reducing hospital readmissions and improving overall patient outcomes.
The seamless exchange of patient data across diverse healthcare providers and systems is fundamental to delivering coordinated, value-based care, a core tenet for companies like Agilon Health. Improvements in health information exchange (HIE) platforms and the growing adoption of standards such as FHIR (Fast Healthcare Interoperability Resources) are directly enhancing this interoperability. This progress is critical for Agilon Health's platform to integrate smoothly with the existing systems of its physician partners, enabling a holistic view of patient histories.
By July 2025, Agilon Health's success hinges on its ability to leverage these technological advancements. For instance, the continued expansion of FHIR adoption, with over 90% of US hospitals reporting EHR adoption by 2024, provides a strong foundation for data sharing. This improved interoperability allows Agilon Health to aggregate patient data more efficiently, supporting their model of managing patient populations and driving better health outcomes through data-driven insights.
Cybersecurity and Data Security
The increasing reliance on digital health technologies and electronic health records (EHRs) by companies like Agilon Health makes robust cybersecurity a critical concern. Protecting sensitive patient data against cyberattacks and breaches is paramount. Agilon Health must continuously invest in advanced security protocols to ensure compliance with evolving regulations and maintain patient trust.
New regulations are anticipated in 2025 specifically targeting data security in healthcare, which will likely increase compliance costs and operational complexities for Agilon Health. A data breach could severely damage Agilon Health's reputation and lead to significant financial penalties. For instance, the healthcare sector experienced a 72% increase in ransomware attacks between 2021 and 2022, highlighting the persistent threat landscape.
- Data Protection Investment: Agilon Health must allocate significant resources towards cybersecurity infrastructure and personnel training to mitigate risks associated with EHRs and digital platforms.
- Regulatory Compliance: Staying abreast of and adhering to new data security regulations, such as those expected in 2025, is crucial for avoiding fines and maintaining operational continuity.
- Patient Trust: Demonstrating a strong commitment to data security is essential for preserving patient confidence and loyalty in an increasingly digital healthcare ecosystem.
- Threat Landscape: The growing sophistication of cyber threats necessitates proactive and adaptive security strategies to protect against evolving attack vectors.
Digital Patient Engagement Tools
The increasing sophistication of digital patient engagement tools, such as AI-powered chatbots and advanced patient portals, is fundamentally reshaping patient-provider interactions within healthcare. These platforms are becoming crucial for empowering individuals with greater autonomy over their health data and facilitating more direct communication channels. For agilon health, leveraging these technologies can significantly enhance patient adherence to prescribed care plans, thereby fostering improved health outcomes and boosting overall patient satisfaction. For instance, a study in 2024 found that patients using digital health tools reported a 25% increase in medication adherence.
agilon health can strategically deploy these digital tools to:
- Enhance patient access to health information and educational resources.
- Streamline appointment scheduling and communication with care teams.
- Facilitate remote monitoring and early intervention for chronic conditions.
- Personalize care journeys and improve patient experience through tailored digital interactions.
Technological advancements, particularly in AI and data analytics, are central to Agilon Health's operational strategy. These tools enable proactive patient risk identification and personalized care management. The global healthcare analytics market's projected growth to $59.1 billion by 2025 underscores the increasing importance of these technologies.
Agilon Health leverages AI for optimizing resource allocation and streamlining administrative tasks, enhancing the efficiency of its value-based care models. Furthermore, the expansion of telehealth and remote patient monitoring (RPM) is crucial, with the global telehealth market expected to exceed $200 billion by 2024, allowing for broader patient reach and improved engagement.
Interoperability, driven by standards like FHIR, is key for Agilon Health to integrate with partner systems, facilitating a comprehensive patient data view. By July 2025, with over 90% of US hospitals adopting EHRs by 2024, improved data sharing capabilities are foundational for Agilon's data-driven insights.
Cybersecurity remains a critical technological factor, with the healthcare sector facing a persistent threat landscape, evidenced by a 72% increase in ransomware attacks between 2021 and 2022. Agilon Health must invest in advanced security to protect sensitive data and maintain patient trust amidst evolving regulations, including those anticipated in 2025.
| Technology Area | Key Advancement/Trend | Impact on Agilon Health | 2024/2025 Data Point |
|---|---|---|---|
| AI & Data Analytics | Predictive modeling for risk stratification | Enables proactive interventions and personalized care plans | Healthcare analytics market projected to reach $59.1 billion by 2025 |
| Telehealth & RPM | Remote patient monitoring and virtual consultations | Expands care access, improves chronic condition management | Global telehealth market projected to exceed $200 billion by 2024 |
| Interoperability | FHIR adoption and HIE platforms | Facilitates seamless data exchange among providers | Over 90% of US hospitals reported EHR adoption by 2024 |
| Cybersecurity | Advanced security protocols and threat mitigation | Protects sensitive patient data and ensures regulatory compliance | 72% increase in healthcare ransomware attacks (2021-2022) |
Legal factors
Agilon Health operates under the strict purview of HIPAA and other data privacy laws, a critical factor given its management of sensitive patient health information. Failure to comply can result in significant penalties, underscoring the need for robust data protection measures.
Anticipated 2025 HIPAA updates are likely to intensify cybersecurity mandates and broaden patient access to their digital health records, potentially requiring Agilon to invest further in platform security and data interoperability.
These regulatory shifts necessitate ongoing vigilance and adaptation in Agilon's data handling practices to maintain compliance and safeguard patient trust.
Agilon Health's operations are significantly shaped by Medicare and Medicaid fraud, waste, and abuse laws. Compliance with the Anti-Kickback Statute, Stark Law, and other federal anti-fraud provisions is paramount to avoid severe penalties. For instance, the Centers for Medicare & Medicaid Services (CMS) reported over $2.1 billion in recovered funds due to fraud and abuse investigations in fiscal year 2023 alone, highlighting the substantial financial and reputational risks of non-compliance.
The legal landscape for value-based care contracts, encompassing models like shared savings, capitation, and risk-based agreements, is intricate and subject to ongoing shifts. Agilon Health's collaborations with physician groups are fundamentally structured around these models, necessitating precise legal drafting to delineate roles, financial terms, and performance benchmarks.
These evolving legal frameworks directly influence Agilon's financial performance and operational strategies. For instance, the Centers for Medicare & Medicaid Services (CMS) regularly updates its models, such as the Medicare Shared Savings Program (MSSP), which impacts potential savings and risk exposure for participating entities. Recent data from 2023 showed that MSSP ACOs generated $5.7 billion in gross savings, with $1.1 billion in net savings, highlighting the financial significance of these regulatory changes.
State-Specific Healthcare Regulations
Beyond federal oversight, Agilon Health must contend with a complex web of state-specific healthcare regulations. These rules, which differ considerably from one state to another, can impact everything from how physician groups are structured to the licensing requirements for healthcare professionals and their permitted scope of practice. Agilon's ability to thrive depends on maintaining a detailed understanding and robust compliance framework tailored to each state where it operates.
Navigating these diverse state laws is crucial for Agilon Health's operational success. For instance, states may have unique requirements for physician network formation or dictate specific data privacy protocols that go beyond federal HIPAA standards. In 2024, as Agilon expanded its reach, staying abreast of these evolving state-level mandates became an increasingly critical component of its business strategy.
- Physician-Group Partnerships: State laws govern the structure and ownership of physician groups, impacting Agilon's partnership models.
- Licensing and Scope of Practice: Variations in state licensing boards and scope of practice rules affect physician employment and service delivery.
- Data Privacy: States may enact data privacy laws stricter than federal regulations, requiring tailored compliance measures for patient information.
- Reimbursement Policies: State-specific Medicaid and commercial payer rules can influence payment rates and contract negotiations.
Telehealth and Digital Health Regulations
The evolving legal framework for telehealth and digital health significantly shapes Agilon Health's operational capabilities and revenue streams. Key regulatory areas include cross-state licensing for healthcare providers, rules governing prescription practices through virtual channels, and stringent data security mandates tailored for digital health platforms.
Federal policy initiatives are actively addressing critical aspects such as payment parity, aiming to ensure telehealth services are reimbursed comparably to in-person visits, and improving access to necessary digital health devices. For instance, the Consolidated Appropriations Act, 2023, extended certain telehealth flexibilities adopted during the COVID-19 public health emergency, providing a more stable regulatory environment.
- Licensing: State-specific licensing requirements can create barriers for Agilon's providers operating across state lines.
- Reimbursement: Payment parity rules directly influence the financial viability of Agilon's technology-enabled service offerings.
- Data Privacy: Compliance with HIPAA and state-specific privacy laws like the California Consumer Privacy Act (CCPA) is paramount for protecting patient data in virtual care.
- Prescribing: Regulations on prescribing controlled substances via telehealth, such as those clarified by the DEA, impact the scope of services Agilon can facilitate.
Agilon Health's adherence to federal and state regulations, particularly regarding data privacy like HIPAA and the CCPA, is fundamental. Anticipated 2025 HIPAA updates will likely bolster cybersecurity requirements and patient data access, compelling further investment in Agilon's digital infrastructure. Non-compliance carries substantial financial and reputational risks, as exemplified by the over $2.1 billion recovered by CMS in FY2023 due to fraud and abuse enforcement.
The company's value-based care models are intrinsically linked to evolving legal frameworks for reimbursement and risk-sharing. Recent successes in programs like the Medicare Shared Savings Program (MSSP), which generated $1.1 billion in net savings for ACOs in 2023, underscore the financial implications of these regulatory shifts. Agilon's strategy must continuously adapt to these dynamic payment policies.
Navigating state-specific healthcare laws, which dictate physician group structures, licensing, and data privacy beyond federal mandates, is crucial for Agilon's multi-state operations. For example, specific state laws might impose stricter data protection measures than HIPAA, requiring tailored compliance solutions. The company's expansion in 2024 necessitated a granular understanding of these varied legal landscapes.
Telehealth regulations, including payment parity and cross-state licensing, directly impact Agilon's service delivery and revenue. The extension of COVID-era telehealth flexibilities through legislation like the Consolidated Appropriations Act, 2023, provides a more stable, albeit evolving, environment for digital health services. Agilon must remain agile to these policy changes to maximize its technology-enabled offerings.
Environmental factors
Climate change poses indirect but significant threats to public health, influencing the demand for healthcare services. For instance, rising global temperatures are linked to an increased incidence of heat-related illnesses, and extreme weather events like hurricanes and floods can lead to injuries, displacement, and the spread of infectious diseases.
Agilon Health, with its focus on senior populations, must consider these environmental shifts. By 2024, the Centers for Disease Control and Prevention (CDC) reported that older adults are particularly vulnerable to the health impacts of climate change, experiencing higher rates of chronic conditions exacerbated by environmental stressors.
These trends, such as potentially more frequent and severe respiratory issues or cardiovascular problems triggered by poor air quality and heatwaves, can directly impact the health outcomes and healthcare utilization patterns of Agilon's patient base. Understanding these long-term public health implications allows for more proactive and effective population health management strategies.
The emergence of public health crises, such as the COVID-19 pandemic, profoundly reshaped healthcare delivery and resource allocation globally. During 2020-2021, telehealth adoption surged by an estimated 300% in some sectors, demonstrating a critical shift in how care is accessed. Agilon Health's capacity to swiftly adapt and bolster its physician partners through these challenging times, perhaps by enhancing telehealth services or remote patient monitoring capabilities, is paramount for sustained success. These events underscore the necessity of robust and flexible healthcare systems designed to effectively navigate widespread health challenges and ensure continuity of care.
The healthcare sector generates substantial environmental waste, from single-use medical supplies and packaging to pharmaceutical byproducts and significant energy usage in facilities. While Agilon Health focuses on technology and services, its operational footprint and the practices of its partner physicians are increasingly subject to environmental scrutiny and the drive for sustainability.
Growing regulatory pressures and public demand for reduced environmental impact within healthcare mean that Agilon's partners may face stricter waste management and disposal requirements. This could influence the adoption of new technologies or processes that minimize waste generation.
Agilon Health's emphasis on efficient, digitally-driven care models can indirectly contribute to sustainability by reducing the need for physical resources and potentially lowering energy consumption associated with traditional healthcare delivery. For instance, telehealth adoption, which Agilon facilitates, can cut down on patient travel emissions and the consumption of disposable materials often used in in-person visits.
The broader push for circular economy principles in healthcare, aiming to reuse and recycle medical equipment and supplies, could also shape Agilon's service offerings and partner engagement strategies. Companies like Medline, a major medical supplier, are investing in sustainability initiatives, aiming to reduce their environmental footprint by 25% by 2030, which reflects the industry's direction.
Access to Healthcare in Geographically Diverse Areas
Geographic dispersion of patients, particularly in rural areas, often presents significant hurdles to accessing consistent primary care. For instance, in 2023, approximately 20% of the U.S. population lived in rural areas, where healthcare provider shortages are more pronounced. Agilon Health's model aims to mitigate these access issues by leveraging its technology platform.
The company's approach facilitates more efficient care delivery, which can be crucial in areas with limited infrastructure or a scarcity of healthcare professionals. This efficiency can translate into better management of chronic conditions and preventative care, even for patients spread across wide geographic distances.
Virtual care capabilities are a key component in Agilon Health's strategy to overcome environmental challenges. By enabling remote consultations and monitoring, Agilon can extend the reach of primary care providers, effectively bridging the gap for patients in geographically diverse settings. This is particularly relevant as telehealth adoption continued to grow, with reports indicating sustained usage in 2024.
- Rural Healthcare Disparities: In 2023, rural areas faced a shortage of over 14,000 primary care physicians, impacting access.
- Agilon's Efficiency Gains: The platform's technology is designed to optimize workflows, potentially reducing administrative burdens and freeing up provider time.
- Virtual Care Expansion: Telehealth services, a core part of Agilon's strategy, saw continued strong adoption in 2024, offering a solution for geographically isolated patients.
- Bridging the Gap: Agilon's model directly addresses the environmental factor of patient dispersion by enabling care delivery beyond traditional brick-and-mortar settings.
Community Health and Environmental Determinants
Community health is significantly shaped by environmental factors like air and water quality, and the availability of green spaces. For Agilon Health, whose model centers on population health management and localized care, addressing these environmental determinants is crucial. Improving these conditions can lead to better patient health and lower long-term healthcare expenditures.
For instance, areas with poor air quality often see higher rates of respiratory illnesses, directly impacting the patient populations Agilon serves. In 2023, the World Health Organization reported that 99% of the global population breathes air that exceeds WHO guideline limits for pollutants. This underscores the direct link between environmental quality and the burden of disease that healthcare providers like Agilon must manage.
- Air Quality Impact: Poor air quality contributes to increased hospital admissions for conditions like asthma and COPD, directly affecting Agilon's patient outcomes and costs.
- Water Quality Concerns: Contaminated water sources can lead to gastrointestinal illnesses and other health issues, requiring more extensive medical intervention.
- Green Space Benefits: Access to parks and recreational areas is linked to improved mental health and increased physical activity, potentially reducing the incidence of chronic diseases.
- Environmental Health Equity: Disparities in environmental quality often fall along socioeconomic lines, highlighting the need for community-focused health strategies to address these inequities.
Environmental factors like climate change and public health crises directly influence healthcare demand and delivery models. Agilon Health must consider how factors such as increased respiratory illnesses due to poor air quality, as reported by the WHO in 2023 affecting 99% of the global population, impact its senior patient base.
The healthcare sector's significant waste generation also presents challenges, with a growing demand for sustainability pushing for stricter waste management. Agilon's digital-first approach, including telehealth adoption which saw significant growth through 2024, can offer an indirect environmental benefit by reducing physical resource consumption.
Geographic dispersion of patients, particularly in rural areas where provider shortages persist (over 14,000 primary care physicians lacking in 2023), is another key environmental consideration. Agilon's platform is designed to enhance care efficiency and extend reach through virtual capabilities, addressing these access hurdles.
Community health is intrinsically linked to environmental quality, such as air and water purity. Agilon's focus on population health means that addressing these determinants, like the 99% of the global population breathing polluted air in 2023, is crucial for improving patient outcomes and managing healthcare costs.
PESTLE Analysis Data Sources
Our PESTLE analysis for agilon health is built on a robust foundation of data from leading healthcare industry reports, government regulatory bodies, and economic forecasting agencies. We integrate insights from market research firms, public health data, and legislative updates to provide a comprehensive view of the macro-environment.
