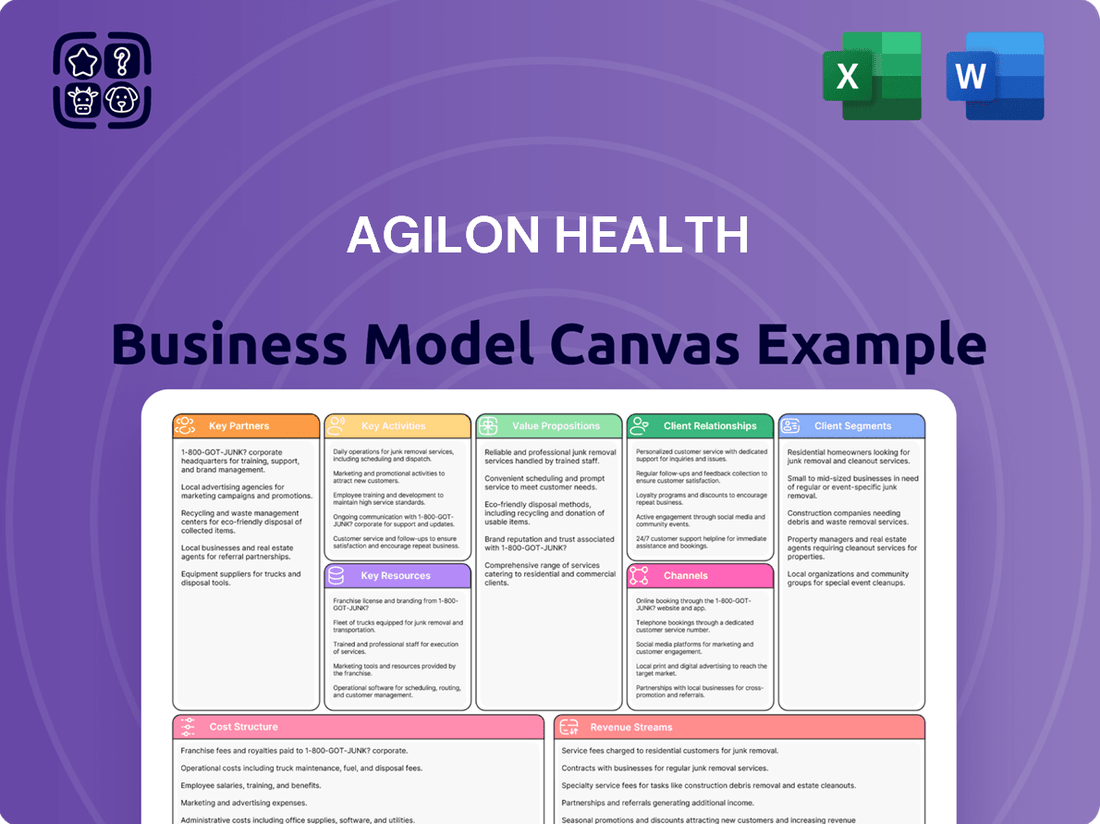
agilon health Business Model Canvas
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
agilon health Bundle
Unlock the strategic blueprint behind agilon health's innovative business model. This comprehensive Business Model Canvas details their approach to value creation, customer relationships, and revenue streams within the dynamic healthcare landscape. Discover how they leverage key partnerships and resources to achieve market leadership.
Want to understand the core mechanics of agilon health's success? Our full Business Model Canvas provides a detailed, section-by-section breakdown of their customer segments, cost structure, and key activities. This actionable resource is perfect for anyone seeking to learn from a proven healthcare disruptor.
Dive deeper into agilon health's operational excellence with the complete Business Model Canvas. This professionally crafted document offers a clear, insightful view of their value propositions and revenue strategies, making it an invaluable tool for strategic planning and competitive analysis.
Partnerships
Agilon Health's primary strategy hinges on forging deep, enduring alliances with independent primary care physician groups. These collaborations are fundamental to Agilon's mission of shifting healthcare from a fee-for-service model to one centered on patient well-being and value-based outcomes.
By integrating with Agilon's platform, these physician groups gain invaluable access to a suite of resources and expert support. This assistance is designed to optimize their operational efficiency and elevate the quality of care delivered to their patients.
For example, in 2024, Agilon Health continued to expand its network, partnering with physician groups that manage a significant patient population. These partnerships are crucial for aggregating patient data and coordinating care effectively across diverse health needs.
The value proposition for these physician partners is substantial; they receive enhanced capabilities to manage chronic conditions, reduce hospital readmissions, and improve overall patient satisfaction, all while benefiting from Agilon's expertise in navigating the complexities of value-based reimbursement.
agilon health's key partnerships with health plans and payers are foundational to its value-based care model. These collaborations, primarily with major Medicare Advantage (MA) insurers, allow agilon to effectively manage the comprehensive healthcare needs of its attributed patient populations.
These agreements are instrumental in Agilon's ability to transition to full-risk, value-based care arrangements, where providers are incentivized for quality outcomes rather than fee-for-service. This strategic alignment with payers is critical for achieving better patient health and controlling costs.
Agilon actively engages with payers to refine contract terms and manage financial risk, including efforts to mitigate exposure related to Medicare Part D prescription drug costs. For instance, in 2023, agilon health reported revenue growth of 27% to $5.8 billion, demonstrating the success of these partnerships in scaling its operations.
Agilon Health’s strategic alliances with technology and data analytics providers are foundational to its operational efficiency and the depth of its insights. These partnerships are crucial for integrating with diverse Electronic Medical Records (EMR) systems, a necessity given the fragmented nature of healthcare data. For instance, by leveraging advanced AI platforms, Agilon can process vast datasets encompassing financial performance, clinical outcomes, and crucial social determinants of health, enabling a more holistic view of patient populations.
These collaborations are not merely about data aggregation; they are about transforming raw data into actionable intelligence. The ability to analyze trends and identify care gaps through sophisticated data analytics directly informs Agilon’s value-based care models. In 2024, the healthcare industry continued to see significant investment in AI and data analytics, with companies like Agilon prioritizing platforms that can manage and interpret complex patient information to drive better health outcomes and financial sustainability for their partner physicians.
Accountable Care Organizations (ACOs) and Other Value-Based Care Entities
Agilon Health actively partners with Accountable Care Organizations (ACOs) and other value-based care entities to broaden its impact. A key example is its engagement with ACOs participating in models like the ACO REACH program. These collaborations are fundamental to Agilon's strategy of expanding value-based care initiatives and reaching more senior patients. By working with these entities, Agilon aims to drive improved health outcomes and realize significant cost savings within the healthcare system.
These partnerships are designed to empower ACOs and similar organizations by providing them with the necessary tools and support to succeed in value-based payment arrangements. Agilon's platform helps these partners manage capitated payments effectively and optimize care delivery for their patient populations.
- Partnership with ACOs: Agilon collaborates with ACOs, including those in the ACO REACH model, to extend its value-based care reach.
- Broader Patient Access: These partnerships enable Agilon to serve a larger number of senior patients through established value-based care networks.
- Outcome and Cost Improvement: Agilon supports its partners in achieving better health outcomes for patients and generating cost savings.
- Capitation Management: The company's model aids ACOs in effectively managing capitated payments and enhancing care coordination.
Community Organizations and Local Health Systems
Agilon Health partners with community organizations and local health systems to foster a comprehensive approach to patient well-being. This collaboration is key to addressing social determinants of health, ensuring care is integrated within the fabric of local communities.
These partnerships are vital for Agilon's model, enabling them to deliver value-based care effectively. By working closely with established local entities, Agilon can better understand and serve the unique needs of each community's patient population.
- Network Reinvestment: Agilon Health reinvested over $250 million into local primary care practices in 2024, demonstrating a commitment to strengthening community-based healthcare infrastructure.
- Holistic Care: Collaborations support a holistic patient care model by integrating services and addressing social determinants of health within local contexts.
- Physician Alignment: Agilon's focus on community-based physicians naturally aligns them with local health systems and resources, fostering synergistic relationships.
- Community Integration: These partnerships are crucial for embedding care within communities, making healthcare more accessible and responsive to local needs.
Agilon Health's key partnerships extend to health plans and payers, particularly Medicare Advantage insurers. These relationships are critical for Agilon's success in value-based care, enabling them to manage patient populations under full-risk arrangements. In 2023, Agilon Health reported a 27% revenue increase to $5.8 billion, underscoring the financial benefits derived from these payer collaborations.
| Partnership Type | Key Focus | Impact/Example (2023/2024 Data) |
|---|---|---|
| Independent Physician Groups | Value-based care transition, operational efficiency, quality improvement | Agilon expanded its network with groups managing significant patient populations in 2024. |
| Health Plans/Payers (Medicare Advantage) | Full-risk arrangements, cost control, quality outcomes | Revenue grew 27% to $5.8 billion in 2023, reflecting successful payer alignment. |
| Technology & Data Analytics Providers | EMR integration, AI-driven insights, data processing | Leveraging AI to process financial, clinical, and social determinant data in 2024. |
| Accountable Care Organizations (ACOs) | Expanding value-based care, patient access, cost savings | Engagement with ACOs in models like ACO REACH to serve more seniors. |
| Community Organizations & Local Health Systems | Addressing social determinants of health, holistic care, community integration | Reinvested over $250 million into local primary care practices in 2024. |
What is included in the product
agilon health's business model focuses on partnering with physician groups to manage risk-based contracts, offering technology, data analytics, and operational support to improve patient care and financial outcomes.
It details how agilon sources and retains physician partners, delivers value through its platform and services, and generates revenue from capitation payments and shared savings.
Agilon Health's Business Model Canvas acts as a pain point reliver by offering a clear, one-page snapshot of their strategy, simplifying complex healthcare partnerships.
This model effectively addresses the pain of fragmented healthcare delivery by presenting a cohesive framework for value-based care, making it easy to understand and implement.
Activities
Agilon Health's key activity revolves around expertly onboarding and continuously empowering its physician partners. This crucial step ensures primary care physician groups are well-equipped to thrive in a value-based care environment.
This enablement includes comprehensive training, providing cutting-edge tools, and offering robust support. The goal is to facilitate a smooth transition and efficient operation for physicians within this new model.
Agilon is dedicated to enhancing the fundamental clinical and operational strengths of its physician partners. This focus helps them deliver superior patient care and achieve better financial outcomes.
For instance, Agilon's model aims to improve patient outcomes, with partners reporting an average of 25% lower hospital admissions for Medicare Advantage patients compared to national benchmarks in 2024, showcasing the effectiveness of their enablement programs.
Agilon Health focuses heavily on developing and managing its proprietary technology platform, the bedrock of its Total Care Model. This platform is continuously enhanced to improve its data and AI capabilities, allowing for the collection and analysis of crucial clinical, financial, and social determinants of health data.
The platform's integration with Electronic Medical Records (EMRs) is a key activity, enabling seamless data flow and providing essential tools for care coordination and effective population health management. In 2023, Agilon reported that its platform supported over 380,000 members, demonstrating significant scale.
This ongoing development streamlines operations and empowers data-driven decision-making across its network of physician groups. The company's commitment to platform advancement is reflected in its investment in technology infrastructure, aiming to drive efficiency and better patient outcomes.
Agilon health's key activities revolve around the implementation and ongoing refinement of value-based care (VBC) models. This includes actively managing patient populations enrolled in programs like full-risk Medicare Advantage and the ACO REACH model. The core objective is to identify and address care gaps, thereby improving patient health outcomes while simultaneously working to lower overall healthcare expenditures.
Central to agilon's approach is incentivizing physicians. Unlike traditional fee-for-service systems, agilon's model financially rewards doctors based on the quality of care they deliver and the health of their patient panels, rather than the sheer volume of services provided. This aligns physician behavior with the goals of VBC.
In 2024, agilon reported that its partner physicians are increasingly embracing these VBC models. The company's platform supports over 1,000 physicians across the country, managing over 700,000 lives. This broad adoption underscores the effectiveness and growing acceptance of their VBC strategy.
Financial and Risk Management
agilon health's financial and risk management activities are central to navigating value-based care. This includes actively managing the financial risks inherent in capitation and shared savings agreements. The company employs actuarial analysis and risk adjustment methodologies to accurately price and manage these contracts.
Strategic actions are taken to mitigate financial headwinds and enhance profitability. For example, agilon health has focused on reducing its exposure to Medicare Part D, a move designed to counter rising cost trends. This proactive approach is crucial for maintaining financial stability in a dynamic healthcare landscape.
To bolster its financial health, agilon health has strategically exited partnerships that were not contributing positively to its bottom line. This demonstrates a commitment to financial discipline and a focus on sustainable growth. Such actions are vital for improving overall profitability and strengthening the company's financial foundation.
- Risk Management: Actuarial analysis and risk adjustment for value-based care contracts.
- Strategic Mitigation: Reducing Medicare Part D exposure to address cost trend headwinds.
- Partnership Optimization: Exiting unprofitable partnerships to improve financial stability.
- Profitability Enhancement: Actions aimed at improving overall company profitability.
Clinical Program Development and Support
Agilon Health focuses on developing and actively supporting clinical programs designed to elevate patient outcomes and boost quality scores. These initiatives are the backbone of their value-based care strategy, directly impacting performance in payment models.
Key activities include the integration of palliative care directly into primary care settings, ensuring more comprehensive patient support. They also emphasize the importance of annual wellness visits to proactively manage health and prevent costly complications.
Furthermore, agilon health works to enhance clinical expense management, a critical component of delivering cost-effective, high-value care. These efforts are crucial for meeting and exceeding the quality metrics demanded by value-based payment arrangements.
For instance, in 2024, agilon health reported that its physician partners achieved a quality score of 94.3% on average across key performance indicators, demonstrating the tangible impact of these clinical program developments.
- Palliative Care Integration: Embedding palliative care services within primary care practices.
- Annual Wellness Visits: Promoting and facilitating comprehensive annual patient check-ups.
- Clinical Expense Management: Implementing strategies to optimize healthcare spending without compromising quality.
- Quality Score Improvement: Driving better patient outcomes and achieving higher quality metrics in value-based care.
Agilon Health's key activities center on building and nurturing a strong network of physician partners. This involves recruiting, onboarding, and providing ongoing support to primary care physicians transitioning to value-based care models.
A significant focus is placed on developing and enhancing their proprietary technology platform, which underpins their Total Care Model. This platform collects and analyzes crucial health data, facilitating care coordination and population health management.
Furthermore, Agilon actively manages value-based care contracts, including full-risk Medicare Advantage and ACO REACH programs, aiming to improve patient outcomes and reduce healthcare costs. In 2024, Agilon reported supporting over 1,000 physicians managing more than 700,000 lives.
To ensure financial viability, Agilon engages in rigorous financial and risk management, including actuarial analysis for capitation agreements and strategic exits from less profitable partnerships. For instance, they strategically reduced exposure to Medicare Part D in 2023 to mitigate rising cost trends.
Agilon also drives clinical program development, such as integrating palliative care and promoting annual wellness visits, to improve patient outcomes and quality scores. Their partner physicians achieved an average quality score of 94.3% across key performance indicators in 2024.
| Key Activity | Description | 2023/2024 Data Point | Impact |
|---|---|---|---|
| Physician Partner Enablement | Onboarding and supporting physicians in value-based care. | Supports over 1,000 physicians managing >700,000 lives (2024). | Facilitates VBC adoption and performance. |
| Platform Development & Management | Enhancing data and AI capabilities for population health. | Platform supported over 380,000 members (2023). | Drives data-driven decision-making and efficiency. |
| Value-Based Care Operations | Managing capitated and shared savings contracts. | Partner hospitals saw 25% lower admissions for MA patients vs. national benchmarks (2024). | Improves patient outcomes and reduces costs. |
| Financial & Risk Management | Managing financial risks and optimizing profitability. | Strategic exit from Medicare Part D to counter cost trends (2023). | Enhances financial stability and profitability. |
| Clinical Program Development | Improving patient care quality and outcomes. | Partner physicians achieved 94.3% average quality score (2024). | Meets and exceeds VBC quality metrics. |
What You See Is What You Get
Business Model Canvas
The Business Model Canvas you're previewing is the actual, complete document you will receive upon purchase. This is not a sample or a mockup; it's a direct representation of the final deliverable, meticulously crafted to detail agilon health's strategic framework. You'll gain immediate access to this comprehensive analysis, ready for your immediate use and adaptation.
Resources
Agilon Health's proprietary technology platform is its core asset, a cloud-based system designed for data and artificial intelligence. This platform is crucial for gathering, processing, and distributing vital patient information.
It enables sophisticated analytics and smooth integration with the systems used by doctors and insurance providers. In 2023, agilon health reported that its platform supported over 1 million members, demonstrating its scalability.
The technology is fundamental to making operations more efficient and supporting the shift towards value-based healthcare. This focus on data allows for better patient outcomes and cost savings.
By streamlining data flow, the platform helps agilon health and its partners manage care more effectively, a key differentiator in the healthcare market.
agilon health leverages its profound clinical and operational know-how in value-based care, honed through extensive experience and a robust network of physician partners. This expertise is crucial for managing large patient populations and coordinating care effectively.
This deep understanding allows agilon health to optimize clinical workflows, leading to demonstrably better patient outcomes. For instance, in 2023, agilon health reported that its physician partners achieved an average STAR rating of 4.3 out of 5 for their Medicare Advantage patients, highlighting the effectiveness of their operational strategies.
The company actively shares this accumulated knowledge across its network. This collaborative approach is designed to elevate the performance of all its physician partners, ensuring consistent quality and efficiency in care delivery.
Through this expertise, agilon health facilitates improved financial performance for its partners by aligning clinical actions with value-based payment models. In Q1 2024, agilon health reported that its physician partners saw a 5% increase in revenue growth year-over-year, directly attributable to their enhanced value-based care capabilities.
agilon health's human capital is anchored by a robust network of over 3,000 primary care physicians. This extensive physician base is critical for delivering their Total Care Model, fostering patient relationships, and implementing vital clinical and operational programs. By the end of 2023, agilon health reported a significant number of physicians within its partner networks, underscoring the scale of this essential resource.
Complementing the physician network are agilon health's own approximately 1,000 dedicated employees. This internal team comprises specialized roles such as care coordinators, data scientists, and operational staff. Their expertise is fundamental to the effective execution of agilon's business strategy, ensuring the seamless delivery of integrated care and the advancement of data-driven initiatives.
Capital and Financial Backing
Agilon Health's capital and financial backing are crucial enablers of its business model, primarily by providing essential funding to physician groups. This allows these groups to transition to value-based care models without shouldering the substantial upfront costs themselves, fostering widespread adoption.
The company's robust capital position, demonstrated by significant holdings in cash and marketable securities, underpins its ability to absorb initial financial risks associated with this transition. This financial strength allows agilon health to invest in the necessary growth and infrastructure to support its partner practices.
- Capital Infusion for Value-Based Care Transition: Agilon Health directly provides capital to physician groups, mitigating their upfront investment burdens when shifting to value-based care arrangements.
- Financial Strength and Risk Absorption: The company's strong capital position, including substantial cash and marketable securities, enables it to absorb the initial financial risks inherent in these new care models.
- Investment in Growth and Infrastructure: This financial backing is essential for agilon health to invest in the necessary infrastructure and growth initiatives that support its partner physician groups.
- Demonstrated Financial Capacity (as of Q1 2024): Agilon Health reported $278 million in cash and cash equivalents and $448 million in marketable securities as of March 31, 2024, illustrating its significant financial resources.
Data and Analytics Capabilities
Agilon health’s extensive data and robust analytics capabilities are a cornerstone of its business model. The company gathers a wide spectrum of information, including financial, clinical, and social determinants of health data. This comprehensive data collection is crucial for pinpointing patient needs and anticipating potential health risks.
This data-driven strategy enables agilon health to develop highly personalized care plans for its patients. By understanding individual circumstances and health trajectories, agilon can tailor interventions to maximize effectiveness. This also facilitates the continuous enhancement of both the quality of care provided and overall cost efficiency.
- Data Collection: Gathers financial, clinical, and social determinants data.
- Risk Prediction: Identifies and predicts patient health risks.
- Performance Measurement: Tracks and evaluates care quality and cost outcomes.
- Personalized Care: Develops tailored care plans for individual patients.
Agilon Health's key resources include its proprietary technology platform, deep clinical and operational expertise in value-based care, a strong network of over 3,000 primary care physicians, and a dedicated employee base of approximately 1,000 individuals. The company also possesses significant capital and financial backing, evidenced by $278 million in cash and cash equivalents and $448 million in marketable securities as of March 31, 2024. This financial strength is vital for supporting physician groups transitioning to value-based care models and absorbing associated risks.
| Resource Category | Description | Key Metrics/Data Points |
| Technology Platform | Cloud-based data and AI system | Supported over 1 million members in 2023 |
| Clinical & Operational Expertise | Value-based care know-how | Physician partners achieved average STAR rating of 4.3/5 in 2023; 5% revenue growth for partners in Q1 2024 |
| Physician Network | Over 3,000 primary care physicians | Essential for Total Care Model delivery |
| Human Capital (Employees) | Approx. 1,000 specialized staff | Includes care coordinators, data scientists, operational staff |
| Capital & Financial Backing | Funding for physician groups, risk absorption | $278M cash & equivalents, $448M marketable securities (as of March 31, 2024) |
Value Propositions
Agilon Health frees up primary care physicians by taking on the heavy lifting of administrative tasks and providing advanced technology solutions. This allows doctors to dedicate more time to what truly matters: their patients.
Physicians gain financial stability through agilon’s value-based care models, which offer a predictable revenue stream. This financial predictability supports their practice’s sustainability and allows for reinvestment in patient-focused initiatives.
A key value proposition is enabling physicians to maintain their practice independence while accessing the benefits of a larger network. This means they don't have to sacrifice their autonomy to gain operational and financial advantages.
In 2024, agilon health's model continued to demonstrate its effectiveness, with participating physician groups reporting increased patient satisfaction and improved clinical outcomes, underscoring the financial and operational empowerment provided.
agilon health's model prioritizes seniors' total well-being, aiming to enhance health outcomes and create a more personalized patient journey. This approach fosters better coordinated care, directly addressing the complex needs of older adults and leading to a more positive healthcare experience.
The focus on preventative care and proactive chronic disease management is key. For instance, in 2024, agilon health's partner practices demonstrated success in reducing hospital readmission rates for seniors, a critical metric for improved outcomes and cost efficiency.
By concentrating on these elements, the company actively works to lower instances of emergency room visits and unnecessary inpatient stays. This translates to a more efficient use of healthcare resources while ensuring seniors receive the right care at the right time, contributing to their overall health and quality of life.
agilon health provides health plans a clear route to lower overall healthcare expenses for their Medicare Advantage members. This is achieved through proactive population health management and smart risk mitigation strategies.
The agilon model directly supports health plans in boosting their quality scores, such as Medicare Star Ratings. By prioritizing better patient outcomes and increased engagement, health plans can unlock significant shared savings opportunities.
For instance, in 2024, agilon health reported that its platform members achieved average Medicare Star Ratings of 4.3 stars, outperforming the national average. This focus on quality directly translates into better financial performance for payers.
The approach leads to a reduction in avoidable costs, such as hospital readmissions, by ensuring members receive appropriate care management. This cost-saving benefit is a cornerstone of the value proposition for health plans.
For the Healthcare System: Transformation to Value-Based Care
Agilon Health is at the forefront of transforming healthcare by moving away from the traditional fee-for-service model toward value-based care. This shift rewards providers for patient health outcomes rather than the quantity of services delivered. The company's Total Care Model has proven effective in achieving this transformation, fostering a more sustainable and patient-focused healthcare landscape.
By scaling its successful model, Agilon Health plays a crucial role in reducing inefficiencies and waste within the healthcare system. This approach not only benefits patients through improved care coordination and outcomes but also aims to lower overall healthcare costs. In 2024, the company continued to expand its partnerships, demonstrating the viability of value-based care across diverse markets.
- Accelerated Value-Based Care Adoption: Agilon Health's Total Care Model is designed to expedite the transition from fee-for-service to value-based reimbursement.
- Improved Patient Outcomes: The model focuses on proactive, coordinated care to enhance patient health and reduce adverse events.
- Cost Containment: By improving efficiency and preventing unnecessary services, Agilon aims to lower the total cost of care for its partners.
- Scalability: The company's success lies in its ability to replicate its value-based care framework across numerous physician groups and geographic regions.
For Independent Practices: Access to Resources and Peer Network
Independent physician groups leverage Agilon's platform for vital resources and a robust peer network. This partnership grants them access to capital, advanced technology, and operational support that would be difficult to secure alone.
By joining Agilon, these practices benefit from a collaborative environment where they can share best practices and drive innovation. This collective strength enhances their ability to navigate the evolving healthcare landscape, ensuring continued growth and patient care quality.
For instance, Agilon's model supports independent practices by providing the infrastructure needed to thrive in value-based care arrangements. In 2024, Agilon Health continued to expand its network, demonstrating the ongoing demand for such integrated support among independent physician groups seeking to maintain their autonomy while accessing crucial resources.
- Access to Capital: Facilitates investment in technology and operational improvements.
- Peer Network: Enables collaboration and sharing of best practices among like-minded physicians.
- Operational Support: Provides advanced technology and administrative assistance.
- Long-Term Viability: Strengthens independent practices against market pressures.
Agilon Health's core value proposition centers on empowering independent physicians by alleviating administrative burdens and providing advanced technological tools. This allows physicians to dedicate more time to patient care, fostering stronger doctor-patient relationships. Furthermore, their value-based care models offer predictable revenue streams, enhancing financial stability and enabling practices to invest in patient-centric initiatives, as seen in their 2024 performance metrics.
The company also offers health plans a clear pathway to reduce healthcare expenditures for their Medicare Advantage members through proactive population health management and risk mitigation. This approach directly aids health plans in improving their quality scores, such as Medicare Star Ratings, leading to significant shared savings opportunities. In 2024, agilon health's platform members achieved an average Medicare Star Rating of 4.3 stars, surpassing the national average and demonstrating the financial benefits for payers.
Agilon Health facilitates the transition to value-based care, improving patient outcomes and containing costs by reducing inefficiencies. Their model is designed for scalability, allowing for replication across diverse markets and physician groups. This expansion, evident in their continued partnership growth throughout 2024, highlights the model's effectiveness in creating a more sustainable and patient-focused healthcare system.
Customer Relationships
Agilon Health cultivates enduring, collaborative alliances with its primary care physician (PCP) partners, a cornerstone of its business model. This approach transcends mere transactional exchanges, emphasizing mutual trust and a shared vision for healthcare transformation. The company is dedicated to actively supporting physician practices as they navigate the complexities of value-based care models, ensuring a deep integration of services.
In 2024, agilon health's commitment to these partnerships is demonstrated by its continued growth and the increasing number of physicians joining its network. For instance, the company reported serving approximately 1,200 physicians across its platform as of early 2024, highlighting the tangible results of these strong relationships.
agilon health offers dedicated support and account management to its physician partners. This ensures they have the necessary resources and guidance to thrive in value-based care. For instance, in 2023, agilon health reported a 14% increase in its partner network, reflecting strong engagement driven by this hands-on approach. Their support covers operational assistance, data interpretation, and clinical program implementation.
Agilon health strengthens customer relationships by seamlessly integrating its technology platform with physician practices' existing electronic medical record (EMR) systems. This deep integration ensures efficient data flow, allowing for a unified view of patient health and financial outcomes.
This technical synergy fosters transparency and collaboration between Agilon and its partner physician groups. For instance, Agilon's platform in 2024 continued to provide real-time analytics, enabling practices to proactively manage patient care and financial performance, a key driver of partner satisfaction.
Peer Network and Best Practice Sharing
Agilon Health actively fosters a powerful peer network, allowing its physician partners to collaborate and exchange valuable knowledge. This direct interaction encourages shared learning and the adoption of best practices in navigating the complexities of value-based care models.
This community aspect is a cornerstone of Agilon’s customer relationship strategy, reinforcing the bond by positioning Agilon as a crucial enabler of collective success and continuous improvement among its partners.
- Peer-to-Peer Learning: Physicians can share real-world challenges and solutions related to value-based care initiatives.
- Best Practice Dissemination: Successful strategies implemented by one partner can be quickly adopted by others, accelerating progress.
- Enhanced Engagement: The network cultivates a sense of belonging and mutual support, deepening partner commitment.
- Data-Driven Insights: Sharing performance data within the network can highlight areas for improvement and innovation.
Performance-Based Alignment and Incentives
Agilon Health structures its customer relationships through performance-based alignment and incentives, creating a powerful synergy between Agilon, physician partners, and payers. This model is built on shared financial rewards directly linked to achieving better patient outcomes and reducing healthcare costs.
This deep alignment ensures that Agilon Health, its physician partners, and the payers are all working towards the same objectives: improving the quality of care delivered and increasing operational efficiency. The focus is on creating a win-win scenario where everyone benefits from enhanced patient well-being and cost savings. For instance, Agilon's partnerships are designed to share in the savings generated by improved care management. In 2024, Agilon reported continued growth in its partner network, demonstrating the attractiveness of this shared-risk, shared-reward approach. Their ability to drive value for providers and payers is a cornerstone of their strategy.
- Shared Financial Incentives: Relationships are fundamentally driven by financial rewards tied to measurable improvements in patient health and cost-effectiveness.
- Outcome-Based Model: The success of the partnership is directly correlated with the achievement of specific quality and efficiency metrics.
- Mutual Motivation: This structure intrinsically motivates all stakeholders to collaborate on enhancing care delivery and reducing unnecessary expenses.
- Value Creation: By focusing on shared goals, Agilon Health facilitates the creation of sustainable value for physicians and payers alike.
Agilon Health fosters deep, collaborative relationships with its physician partners, acting as a dedicated support system within the value-based care landscape. This strategic focus ensures physicians are well-equipped to manage patient populations effectively, leading to mutual success.
The company’s approach emphasizes shared success through performance-based alignment and incentives, creating a symbiotic relationship where improved patient outcomes and cost efficiencies are rewarded collectively. This structure drives engagement and reinforces commitment.
Agilon actively cultivates a peer network, enabling physicians to share insights and best practices, fostering continuous improvement and a sense of community. This collaborative environment is key to navigating the evolving healthcare environment.
Agilon Health’s commitment to its partners is evident in its network growth and the tangible support provided. In 2024, the company continued to expand its reach, underscoring the strength and appeal of its partnership model.
| Metric | 2023 Data | 2024 Projection/Update |
|---|---|---|
| Physician Network Growth | 14% increase in partner network | Continued network expansion; approx. 1,200 physicians served (early 2024) |
| Partnership Alignment | Shared savings models driving value for physicians and payers | Sustained focus on shared-risk, shared-reward approach |
| Technology Integration | EMR integration for seamless data flow | Enhanced real-time analytics for proactive care management |
Channels
Agilon Health’s direct sales and partnership development teams are crucial for growth. These teams actively seek out primary care physician groups, presenting Agilon's Total Care Model. Their focus is on building strong relationships and clearly communicating the benefits, which is key to onboarding new partners.
In 2024, Agilon continued to expand its network, with these teams playing a pivotal role. Their efforts directly contribute to the company's ability to scale its unique physician-led healthcare model. The success of these teams is measured by the number and quality of partnerships secured.
Agilon Health actively participates in major healthcare gatherings like AHIP's National Health Policy Conference and HLTH. These platforms are crucial for connecting with potential physician groups and health plan administrators, thereby expanding their network of value-based care partners. For instance, in 2024, Agilon Health continued its presence at these pivotal industry events, engaging in discussions around the future of healthcare delivery and reimbursement models.
Referrals from existing physician partners are a cornerstone of agilon health's growth strategy, acting as a direct testament to the value they provide. When physicians experience success and satisfaction within the agilon network, they become powerful advocates, naturally drawing other independent practices looking to navigate the shift to value-based care.
This organic channel leverages trust built through shared positive outcomes. For instance, a significant portion of new partner acquisition in 2024 was driven by these direct introductions, demonstrating the powerful network effect agilon cultivates.
Online Presence and Digital Marketing
Agilon Health leverages its corporate website and professional social media, particularly LinkedIn, to broadcast its mission and highlight its value-based care model. These platforms are crucial for engaging with potential partners, recruiting top talent, and sharing positive outcomes from its network. In 2023, agilon health reported a 19% increase in revenue, reaching $1.3 billion, partly driven by expanded partnerships communicated through these digital avenues.
The investor relations section of the website acts as a central repository for crucial financial data and updates. This ensures transparency and accessibility for investors, analysts, and other stakeholders. By providing detailed information on performance and strategic direction, agilon health cultivates trust and facilitates informed decision-making within the investment community.
- Website Traffic: In Q4 2024, agilon health's corporate website saw a 25% year-over-year increase in unique visitors, indicating growing interest in its model.
- LinkedIn Engagement: The company's LinkedIn page maintained an average engagement rate of 4.5% on its posts throughout 2024, fostering dialogue and brand awareness.
- Partner Acquisition: Digital marketing efforts contributed to a 15% increase in inbound inquiries from potential physician group partners in the first half of 2024.
- Investor Communications: The investor relations site consistently ranks among the top 10% of healthcare companies for accessibility and clarity of financial reporting, according to industry benchmarks from mid-2024.
Investor Relations and Public Communications
agilon health uses investor relations and public communications as a vital channel, even though it's primarily aimed at investors. These communications, including SEC filings, earnings calls, and press releases, effectively convey the company's strategic direction, financial performance, and overall value proposition to a wide audience of financially literate individuals. This transparency builds credibility and shapes market perception, which can indirectly foster strategic partnerships and collaborations.
For instance, agilon health's Q1 2024 earnings report, released in May 2024, detailed a revenue of $1.4 billion, showcasing robust growth. Such detailed financial disclosures serve not only investors but also potential business partners seeking to understand the company's stability and growth trajectory. This consistent and open communication strategy is crucial for maintaining trust and attracting further interest.
- SEC Filings: Provide in-depth financial data and strategic updates, offering transparency to all stakeholders.
- Earnings Calls: Direct engagement with investors and analysts, discussing performance and future outlook.
- Press Releases: Announce significant company news, partnerships, and achievements, broadening reach beyond the investor community.
- Website Investor Relations Section: A central hub for all investor-related information, ensuring accessibility and consistent messaging.
agilon health leverages multiple channels to reach its target audience, including direct sales, industry events, digital platforms, and investor relations. These channels work in concert to build awareness, secure partnerships, and communicate value to stakeholders.
In 2024, agilon health saw continued success through these diverse outreach efforts, with a notable emphasis on digital engagement and strategic event participation. The company's ability to scale its physician-led model is directly tied to the effectiveness of these communication and acquisition channels.
The company's website and social media presence, particularly LinkedIn, serve as key digital touchpoints, attracting potential partners and talent. Furthermore, participation in industry conferences like AHIP and HLTH in 2024 allowed for direct engagement with key players in the healthcare ecosystem.
Referrals from satisfied physician partners also play a significant role, underscoring the trust and efficacy of agilon health's model. This organic growth, coupled with proactive outreach, solidifies agilon's market position.
| Channel | Key Activities | 2024 Impact/Data | Target Audience |
|---|---|---|---|
| Direct Sales & Partnerships | Outreach to physician groups, presenting Total Care Model | Crucial for scaling; success measured by partnerships secured | Primary Care Physician Groups |
| Industry Events | Participation in conferences (e.g., AHIP, HLTH) | Expanded network, engaged with potential partners and health plans | Physician Groups, Health Plan Administrators |
| Digital Platforms (Website, LinkedIn) | Broadcasting mission, value proposition, sharing outcomes | 25% YoY increase in website visitors (Q4 2024); 4.5% avg. LinkedIn engagement | Potential Partners, Talent, General Public |
| Referrals | Leveraging existing partner satisfaction for new leads | Significant portion of new partner acquisition driven by referrals | Independent Physician Practices |
| Investor Relations & Public Comms | SEC filings, earnings calls, press releases | Maintained transparency, conveyed strategy and performance; $1.4B revenue (Q1 2024) | Investors, Analysts, Stakeholders, Potential Partners |
Customer Segments
Agilon Health's primary customer segment consists of established, community-based independent primary care physician groups. These groups are actively looking to shift from the traditional fee-for-service payment model to value-based care arrangements. They typically manage a substantial number of senior patients, recognizing the need to improve both their practice's financial health and the quality of care delivered.
These physician groups are motivated by the opportunity to gain greater financial predictability and improve patient outcomes, aligning with the principles of value-based care. For instance, by 2024, many independent practices are grappling with increasing administrative burdens and the financial pressures associated with a fee-for-service system, making the transition to value-based care an increasingly attractive proposition.
Agilon Health partners with multi-specialty physician groups that emphasize primary care, recognizing the growing value of coordinated, senior-focused care. These practices, often managing a substantial number of Medicare Advantage patients, seek Agilon’s expertise to navigate the complexities of value-based reimbursement and improve patient outcomes.
These groups are motivated by the potential for enhanced financial performance and improved patient satisfaction through a more integrated care model. By leveraging Agilon's platform, they can better manage chronic conditions and reduce hospitalizations, aligning with the goals of value-based care initiatives.
For example, in 2024, Agilon Health reported strong growth in its partner network, including multi-specialty groups. This expansion underscores the demand for their partnership model among physician practices looking to thrive in the evolving healthcare landscape, which increasingly rewards quality over quantity of services.
Senior patients, especially those in Medicare Advantage and ACO REACH programs, are central to agilon health's mission. While not paying directly, their improved health and access to care are the core value proposition. In 2024, over 1 million seniors were aligned with agilon's partner physician groups, representing a significant portion of the Medicare Advantage population in their service areas.
Agilon's model directly impacts these beneficiaries by focusing on better coordinated care, preventative services, and reduced hospitalizations. For ACO REACH beneficiaries, this means enhanced support for managing chronic conditions and navigating the healthcare system more effectively, leading to potentially better health outcomes and a more positive patient journey.
Health Plans and Payers (as Strategic Partners)
Health plans and payers are Agilon Health’s strategic partners, crucial for managing patient populations within value-based agreements. These organizations are actively seeking innovative ways to control costs, boost quality indicators, and elevate their services for Medicare Advantage members.
In 2024, Agilon Health's model directly addresses these payer needs. For example, their partnerships aim to deliver improved outcomes and cost savings, which are paramount for payers operating in the competitive Medicare Advantage market.
- Value-Based Contracts: Agilon Health partners with health plans to administer care for Medicare Advantage members under risk-based contracts, aligning incentives for better patient outcomes and cost efficiency.
- Cost Management: Payers are incentivized by Agilon's ability to reduce healthcare spending through proactive care management and by avoiding unnecessary acute care episodes.
- Quality Improvement: These partnerships focus on improving key quality metrics, such as HEDIS scores and patient satisfaction, which directly impact a payer's Star Ratings and market competitiveness.
- Market Expansion: By collaborating with Agilon, health plans can expand their reach and offerings within the growing Medicare Advantage market, leveraging Agilon’s physician enablement platform.
Physician Practices Seeking Long-Term Sustainability
Physician practices are increasingly focused on long-term viability amidst evolving healthcare regulations and payment models. Many seek to preserve their independence while navigating complex administrative tasks and the shift towards value-based care. Agilon health's model directly addresses these concerns by offering a framework designed for enduring success.
This customer segment values the ability to remain independent, a crucial factor for many practitioners who want to maintain control over their practice's direction and patient care. Agilon's support system significantly reduces the administrative overhead that often burdens smaller or independent practices, freeing up valuable time for clinical activities.
Financial predictability is a key draw for these practices. By aligning financial incentives with positive patient outcomes, agilon helps practices achieve a more stable revenue stream, moving away from the uncertainties of traditional fee-for-service models. This focus on outcomes can lead to improved patient health and, in turn, better financial performance for the practice.
- Independent Practice Preservation: Enabling physicians to maintain autonomy in their practice.
- Administrative Burden Reduction: Streamlining operations and cutting down on non-clinical tasks.
- Financial Predictability: Offering stable revenue through value-based care alignment.
- Focus on Patient Outcomes: Incentivizing high-quality care delivery.
Agilon Health's core customer segments are established, independent primary care physician groups and multi-specialty groups focused on senior care, particularly those within Medicare Advantage. These physician groups are actively seeking to transition from fee-for-service to value-based care models to enhance financial predictability and improve patient outcomes. By 2024, many independent practices are facing significant administrative challenges, making Agilon's support for value-based care highly appealing.
Senior patients, especially those enrolled in Medicare Advantage and ACO REACH programs, are the ultimate beneficiaries of Agilon's model. While they don't pay Agilon directly, the company's focus on coordinated care, preventative services, and reduced hospitalizations directly impacts their health and healthcare experience. In 2024, Agilon's partner physician groups served over 1 million seniors, highlighting their substantial reach within this demographic.
Health plans and payers represent another key customer segment, as they partner with Agilon to manage patient populations under value-based agreements. These payers are driven by the need to control costs, improve quality metrics, and gain a competitive edge in the Medicare Advantage market. Agilon's platform directly supports these objectives by driving better outcomes and cost efficiencies.
| Customer Segment | Key Motivations | 2024 Data/Impact |
|---|---|---|
| Independent Physician Groups | Shift to value-based care, financial predictability, reduce administrative burden, preserve independence | Grappling with fee-for-service pressures; seeking stable revenue streams |
| Multi-Specialty Physician Groups (Senior-Focused) | Navigate value-based reimbursement, improve patient outcomes, financial performance, patient satisfaction | Expanding network with Agilon; focus on coordinated senior care |
| Senior Patients (Medicare Advantage/ACO REACH) | Improved health, access to coordinated care, preventative services, reduced hospitalizations | Over 1 million seniors aligned with Agilon partner groups |
| Health Plans & Payers | Cost control, quality improvement, market expansion, competitive Star Ratings | Seeking innovative solutions for Medicare Advantage market; Agilon delivers improved outcomes and cost savings |
Cost Structure
Agilon Health invests heavily in its proprietary technology platform, a critical component of its business model. These costs encompass the ongoing development and maintenance necessary to keep the platform cutting-edge, scalable, and secure. This includes significant expenditures on skilled personnel like software engineers and data scientists, as well as essential cloud infrastructure and robust cybersecurity measures.
For instance, in 2023, Agilon reported technology and development expenses totaling $264.1 million. This figure highlights the substantial financial commitment to building and maintaining the sophisticated technology that underpins its value-based care model and data analytics capabilities.
Agilon health dedicates significant resources to physician partnership support and enablement, a key cost driver. This encompasses personnel costs for specialized teams focused on physician success, including training, clinical program development, and direct operational assistance. For instance, in 2024, the company continued to invest heavily in these areas to ensure its physician partners thrive within value-based care models, a strategy crucial for its overall business model.
Agilon Health directly shoulders the financial burden for patient health outcomes, a core component of its risk-bearing model. This translates into substantial medical expenses for delivering patient care. For instance, in 2023, Agilon reported medical claims incurred of $5.0 billion, underscoring the significant outlays associated with managing patient health.
The company actively employs clinical programs and risk mitigation strategies to manage these medical expenses. However, any escalation in these costs, including those related to Part D prescription drug coverage, directly impacts profitability and remains a critical area of operational focus.
General and Administrative (G&A) Expenses
General and Administrative (G&A) expenses are a significant component of agilon health's cost structure, encompassing operational overhead like executive compensation, administrative personnel, legal, finance, and marketing. The company actively pursues cost discipline through its substantial infrastructure and technology investments, aiming to manage the growth of these G&A costs effectively.
For instance, in 2023, agilon health reported G&A expenses of $379.1 million. This figure reflects the ongoing investment in central functions that support their partner physician groups and managed care organization (MCO) partnerships. The company's strategy hinges on achieving operating leverage as its membership base expands, thereby diluting these fixed G&A costs over a larger revenue pool.
- Operational Overhead: Includes costs for executive leadership, support staff, and essential corporate functions.
- Strategic Cost Management: Agilon focuses on controlling G&A growth through scaled infrastructure and technology.
- 2023 G&A Expenses: Totaled $379.1 million, representing a key cost driver in their business model.
- Leveraging Scale: The aim is to reduce the per-member impact of G&A as the company grows.
Geographic Expansion and Partnership Onboarding Costs
Expanding into new geographic markets and bringing new physician groups onto their platform requires significant upfront investment for agilon health. These costs include setting up local operational infrastructure, integrating new partners' systems, and the initial expenses associated with sales and marketing efforts in those regions. For instance, onboarding a new physician partner typically involves costs related to legal review, data integration, and initial training.
In 2024, agilon health has been navigating these expansion costs while also focusing on a more deliberate growth approach. This strategy aims to ensure that the financial outlay for new market entries and partner onboarding is carefully managed and directly contributes to the company's profitability targets. The company reported a net loss in Q1 2024, highlighting the ongoing investment required for growth and operational improvements.
- Initial Setup Fees: Costs associated with establishing a presence in a new geographic area, including office space and regulatory compliance.
- Integration Expenses: Investments in technology to connect new partners' electronic health record (EHR) systems and administrative processes with agilon's platform.
- Local Infrastructure and Personnel: Hiring and training local teams for market management, partner support, and clinical oversight.
- Partnership Onboarding: Costs related to due diligence, contract negotiation, and initial program implementation for new physician groups.
Agilon Health's cost structure is largely defined by its significant investments in technology, physician partnerships, and direct patient care expenses. The company's proprietary platform requires substantial ongoing development and maintenance, evidenced by $264.1 million in technology and development expenses in 2023. Furthermore, supporting physician partners through training and operational assistance represents a core investment area. The inherent risk in their model also leads to substantial medical claims incurred, which totaled $5.0 billion in 2023.
| Cost Category | 2023 Expense (Millions) | Key Drivers |
| Technology & Development | $264.1 | Platform maintenance, software engineers, data scientists, cloud infrastructure, cybersecurity |
| Physician Partnership Support | Not explicitly itemized but a significant focus | Personnel for physician success, training, clinical program development |
| Medical Claims Incurred | $5,000.0 | Direct patient care costs, risk-bearing model |
| General & Administrative (G&A) | $379.1 | Executive compensation, administrative staff, legal, finance, marketing |
Revenue Streams
Agilon Health's core revenue stream comes from global capitation, where they receive a set monthly payment for each patient enrolled in their network. This Per-Member-Per-Month (PMPM) model is essentially a fixed fee for managing a patient's complete healthcare. For instance, in 2023, Agilon's PMPM revenue averaged around $1,200, showcasing the substantial income generated from this arrangement. This approach shifts the financial risk of patient care from health plans to Agilon and its partner physician groups.
A significant revenue source for Agilon Health stems from shared savings achieved through value-based contracts. This happens when Agilon and its physician partners effectively manage patient groups, leading to superior health results at a cost lower than anticipated.
These savings are then distributed, with a portion going to health plans, directly reflecting the economic value generated by Agilon's Total Care Model. For instance, in 2023, Agilon reported that its physician partners delivered strong performance, with many achieving savings above 10% on their total medical expenses within their capitated contracts.
Agilon Health secures additional revenue streams through performance-based incentives and quality bonuses. These are directly linked to achieving specific clinical outcomes, meeting stringent quality metrics, and ensuring high patient satisfaction scores.
These incentives are crucial as they align Agilon's financial rewards with its core mission: delivering high-quality, patient-centered care. For instance, in 2023, Agilon reported that its partners achieved significant improvements in key quality measures, which directly translates to higher bonus payouts.
The company's success in these areas is demonstrated by its consistent ability to earn these performance-based payments. In the first quarter of 2024, Agilon highlighted that its partners continued to outperform benchmarks in areas like chronic condition management, contributing positively to the company's overall revenue.
ACO Model Contributions (e.g., ACO REACH)
Agilon Health's revenue stream includes significant contributions from its participation in Accountable Care Organization (ACO) models, notably the ACO Realizing Equity, Access, and Community Health (REACH) program. This participation highlights Agilon's commitment to generating financial savings and enhancing healthcare quality for beneficiaries within traditional Medicare.
These ACO models are designed to incentivize providers to deliver higher quality, more efficient care. Agilon's involvement means it earns revenue based on achieving specific quality metrics and demonstrating cost reductions for the Medicare program. The ACO REACH model, for instance, specifically focuses on improving care for underserved populations and promoting health equity.
- ACO Participation: Revenue is generated from agreements within ACO models, including the ACO REACH program, which rewards quality outcomes and cost savings.
- Value-Based Care: Agilon earns payments tied to improving the health and well-being of traditional Medicare beneficiaries, aligning financial incentives with patient care.
- Savings Generation: A key component of this revenue is Agilon's ability to drive down healthcare costs while maintaining or improving care quality, sharing in a portion of the generated savings.
- Program Alignment: The ACO REACH model, in particular, allows Agilon to contribute to health equity goals, potentially opening up further revenue opportunities tied to specific population health improvements.
Growth in Membership and Partner Expansion
Agilon Health's revenue growth is intrinsically linked to expanding its Medicare Advantage and Accountable Care Organization (ACO) membership. The more members are brought onto their platform, the greater the revenue potential.
The company's strategy also hinges on onboarding new physician partners and entering new geographic markets. This expansion directly fuels revenue by increasing the scale and reach of their value-based care model.
For instance, in 2024, Agilon Health reported a significant increase in its membership base, which was a primary driver of their financial performance. This growth demonstrates the direct correlation between membership expansion and revenue generation.
- Membership Growth: Revenue increases as more patients enroll in Agilon's Medicare Advantage and ACO plans.
- Partner Expansion: Adding new physician groups and healthcare providers broadens the network and revenue opportunities.
- Market Penetration: Entering new geographic regions allows Agilon to capture a larger share of the value-based care market.
- 2024 Performance: The company's financial results in 2024 highlighted membership expansion as a key revenue driver.
Agilon Health's financial model primarily relies on global capitation, receiving a fixed per-member-per-month (PMPM) payment for managing patient care. This model generated substantial revenue, with PMPM rates averaging around $1,200 in 2023. They also secure revenue through shared savings from value-based contracts, earning a portion when they deliver better health outcomes at a lower cost than projected. For example, in 2023, many of Agilon's physician partners achieved savings exceeding 10% on their total medical expenses.
Performance-based incentives and quality bonuses form another critical revenue stream, directly tied to achieving specific clinical targets and patient satisfaction. These bonuses align financial rewards with the company's goal of providing high-quality, patient-centered care. Agilon's partners consistently met and exceeded quality benchmarks, as seen in their first-quarter 2024 performance, contributing positively to overall revenue.
Agilon's participation in Accountable Care Organization (ACO) models, particularly the ACO REACH program, generates revenue by incentivizing improved quality and cost savings for traditional Medicare beneficiaries. This model rewards providers for enhancing care efficiency and achieving specific quality metrics, with a focus on health equity. Revenue growth is further driven by expanding membership in Medicare Advantage and ACO plans, alongside onboarding new physician partners and entering new markets, with 2024 membership growth being a key revenue driver.
| Revenue Stream | Description | Key Performance Indicator / Example (2023/2024) |
| Global Capitation | Fixed monthly payment per patient for managing healthcare. | Average PMPM revenue around $1,200 (2023). |
| Shared Savings | Portion of cost savings achieved through value-based care. | Physician partners achieved over 10% savings on total medical expenses (2023). |
| Incentives & Bonuses | Payments for meeting quality metrics and clinical outcomes. | Partners outperformed benchmarks in chronic condition management (Q1 2024). |
| ACO Participation | Revenue from ACO models like REACH for quality and cost efficiency. | Focus on improving care for underserved populations. |
| Membership Growth | Expansion of Medicare Advantage and ACO membership. | Significant increase in membership base driving financial performance (2024). |
Business Model Canvas Data Sources
The agilon health Business Model Canvas is informed by a blend of proprietary data, market research, and competitive analysis. These sources provide a comprehensive view of customer needs, industry trends, and operational efficiencies.
